Explicit safeguards wanted for 12-month prescribing for Māori
For 12-month prescribing to be safe for Māori explicit safeguards are needed, Te Tiratū Iwi Māori Partnership Board says in a Position Statement authored by pharmacist Leanne Te Karu.
Ensuring barriers to access are recognised and removed is key, rather than reduced Māori engagement with their prescriber and medicines by way of a longer prescribing period.
The extended period will work well if it reduces routine GP visits for people with stable conditions, easing pressure on primary care services, but may not provide the same benefits to Māori Tiratū chief executive Brandi Hudson says.
Lighter paperwork, or better care?
A change to prescription time-frames isn’t a win for all whānau, writes Brandi Hudson.
I understand why some people welcomed the policy change extending the prescribing period to 12 months. It means fewer repeat appointments. Less admin. Less cost. More convenience.
But where I work, at Te Tiratū Iwi Māori Partnership Board, we’re deeply concerned.
Without strong equity and safety safeguards, this change risks widening Māori health inequities, increasing under-care, delaying diagnosis, and causing medication-related harm.
The policy itself sounds tidy. Prescribers can issue prescriptions for up to 12 months for some medicines, while dispensing at the pharmacy still occurs in maximum three-monthly periods. Controlled drugs are excluded. It’s framed as a way to reduce unnecessary appointments and ease pressure on the system.
The trouble is, medicines sit inside real lives. And for many whānau, those lives include multiple conditions, inconsistent access to care, and long gaps between clinical reviews.
It’s easy to imagine a “stable patient” who takes one medicine and has no complications as the basis for policy change. But many of our whānau are managing complex comorbidities, such as diabetes alongside asthma, cardiovascular disease alongside kidney issues, chronic pain alongside depression, and respiratory illness alongside poverty-related stress. Even the presence of two conditions can create risks, interactions, and side effects that need regular review.
For those whānau, prescribing is not just a matter of being told: “Here’s your tablets for the year.” The prescription is part of a care plan that should include monitoring, blood tests, screening, follow-up, and the chance to adjust treatment before harm occurs.
That’s why Te Tiratū supports reducing barriers, but we can’t support a change that reduces the number of touchpoints without putting in place safeguards to protect those who are already missing out.
Māori face significant barriers to accessing medicines. Despite higher rates of chronic conditions such as diabetes, cardiovascular disease and respiratory illness, Māori are overall less likely than non-Māori to access dispensed medicines. In some cases, prescriptions aren’t collected at all because cost, transport, and system barriers make it too difficult.
Extending the length of a prescription doesn’t automatically fix those issues. In some cases, it could even mask them. On paper, a person might look “covered” for 12 months. In reality, they might still be missing doses, skipping follow-ups, not getting blood tests done, or deteriorating quietly until they end up in hospital.
There’s another risk we need to talk about honestly, and that’s the assumption of “clinical stability”.
Who will get labelled stable enough for a 12-month prescription? And who won’t?
In a health system where bias can shape decision-making, sometimes unconsciously, our whānau may be less likely to receive careful follow-up, or more likely to be deemed “fine” without the monitoring that should come with long-term medicines.
Māori don’t experience ill-health in isolation. We live with higher rates of the country’s top five killers — cancer, diabetes, heart disease, stroke and respiratory illness — often all at once. These conditions don’t arrive one by one. They stack, interact, and compound over time.
Add to this the realities many whānau face, such as not always having enough kai, stable housing, or financial security. These are not side issues — they directly affect whether medicines are taken as prescribed, whether follow-up appointments are kept, and whether pain or deterioration is noticed early.
For many of our whānau, poor oral health and chronic foot problems are not minor inconveniences. They affect mobility, sleep, ability to work, and self-esteem. Pain becomes normal. Limited mobility becomes normal. Struggling through becomes normal.
And when complexity becomes normal in a health system under strain, it can quietly slip through the cracks.
Instead of prompting closer monitoring, long-term medicines and complex conditions can be treated as “baseline”. Symptoms are more likely to be interpreted as expected rather than concerning. Whānau may be assessed as “stable” or “fine” not because they’re well, but because their level of unwellness has been unconsciously normalised.
This is how bias can operate without intention. Not through overt neglect, but through lowered expectations of recovery, stability, and follow-up.
Equity in healthcare doesn’t mean treating everyone the same. It means recognising when people are carrying more medical, social, and economic burdens, and responding with more care, not less.
Dr Leanne Te Karu, our expert advisor, has warned that reducing prescribing touchpoints can reduce opportunities to detect deterioration, review side effects, adjust treatment, or optimise medicines. And while community pharmacists are essential, they can’t replace comprehensive clinical review and diagnostic reassessment.
That’s why the solution isn’t simply to provide longer prescriptions. The solution is to build stronger systems around them.
We need national guidance on who isn’t clinically-appropriate to receive a 12-month prescription, and we need equity-focused monitoring that shows what is happening for Māori, not just what is happening on average across the whole population.
We need transparent reporting of adverse events, hospitalisations, medication changes, and wastage. We need Māori-led evaluation of safety, trust, communication and cultural safety.
Most importantly, we need to stop treating medicines as isolated clinical decisions and start treating them as part of a Treaty-aligned system of care.
Te Tiriti obligations of partnership, equity and active protection aren’t optional extras. Partnership means Māori are involved in designing and governing the processes that provide access to medicines, not merely consulted after decisions are made.
Equity means Māori achieve the same access to subsidised medicines and support services as everyone else, with real-world barriers like transport and culturally appropriate information addressed directly. Active protection means outcomes for Māori are monitored, and the policy is adjusted quickly if harm is emerging.
There is a better way forward. Māori pharmacy experts like Dr Te Karu have long advocated for a Te Tiriti-aligned strategy, grounded in Pae Ora and mātauranga Māori, to bring all the right expertise into the room and design medicines pathways that reflect whānau realities, not just administrative convenience.
A 12-month prescription might reduce hassle. But it won’t keep you well if the system stops checking in.
If we want this change to succeed for whānau, we have to measure success by whether Māori are safer, healthier, and better supported — not whether the paperwork got lighter.
Brandi Hudson (Ngāti Maniapoto, Ngāti Rarua, Ngāti Pikiao) is the tumu whakarae (chief executive) of Te Tiratū Iwi Māori Partnership Board, providing strategic leadership across the Waikato rohe to strengthen Māori influence in health system design, planning and service delivery.
She has held senior roles across community, government and not-for-profit sectors, including inaugural CEO of the Independent Māori Statutory Board in Auckland.
Gaps remain in Māori health
The Waikato Local has covered Te Tiratū Iwi Māori Partnership Board’s warning about the 12-month prescription medicine policy change and its potentially adverse impact on whānau Māori as outlined in our Position Statement.
No safeguards for 12-Month prescriptions, Māori health leaders warn
Brandi Hudson, Te Tiratū Tumu Whakarae is warning the Government’s move to 12-month prescriptions could deepen under-care and widen health inequities for whānau Māori unless strong safeguards are built in from day one. Speaking with Waatea she says longer scripts may suit some, but without proper monitoring and follow-up they risk fewer check-ins, delayed diagnosis and worsening long-term conditions. The board is calling for mandatory review points, proactive follow-up systems, culturally safe pathways designed with Māori providers, and real-time data oversight given the policy took effect on 1 February 2026.
12-Month prescriptions risk widening Māori health inequities without safeguards
MEDIA STATEMENT
FOR IMMEDIATE RELEASE
Friday 30 January 2026, 4:00 PM
2 minutes to Read

Te Tiratū Iwi Māori Partnership Board is warning that the introduction of 12-month prescriptions from 1 February 2026 risks increasing under-care, delayed diagnosis, and medicine-related harm for Māori unless strong equity and safety safeguards are put in place.
While Te Tiratū supports efforts to reduce barriers for whānau, Te Tiratū Tumu Whakarae, Brandi Hudson says affordability and convenience alone do not guarantee safe or equitable access to medicines.
“From a Hauora Māori perspective, access to medicines is not a single transaction, it is a continuous pathway of care,” she said. “Any policy change must actively uphold Te Tiriti o Waitangi obligations of partnership, equity and active protection.”
“Partnership means Māori are involved in designing and governing medicines access pathways, not just consulted after decisions are made. Equity requires ensuring Māori have the same access to subsidised medications and support services as others, addressing barriers like transport or culturally appropriate information. Active protection involves monitoring outcomes for Māori and adjusting policy to prevent under-care or delayed treatment,” she said.
The legislative change will allow prescribers to issue prescriptions covering up to 12 months for some medicines, with dispensing continuing in maximum three-monthly periods. Controlled drugs are excluded.
Māori already face significant barriers to accessing medicines. Despite higher rates of chronic conditions such as diabetes, cardiovascular disease, and respiratory illness, Māori are overall less likely to access dispensed medicines than non-Māori.
In some cases, prescriptions are not collected at all due to cost, access, and system barriers. These inequities mean that extending prescription duration alone will not ensure medicines safely reach whānau who need them most.
Dr Leanne Te Karu, expert advisor to Te Tiratū and author of its Tauāki Tū Position Statement on this policy change, says it carries significant risk if implemented without explicit safeguards.
“Māori already experience lower rates of monitoring, fewer proactive clinical reviews, and later diagnosis of chronic and complex conditions,” she said.
“Reducing prescribing touchpoints risks further decreasing opportunities to detect deterioration, review side effects, adjust treatment, or optimise medicines.”
Dr Te Karu warns that assumptions about “clinical stability” may be unsafe in contexts where care is fragmented, monitoring is inconsistent, and social and economic pressures affect medicine use.
“Prescriber discretion and unconscious bias can shape who is deemed ‘stable’.”
“Longer prescription intervals may be framed as empowerment when they instead reflect system withdrawal or under-service. Community pharmacists play a vital role, but they cannot replace comprehensive clinical review and diagnostic reassessment.”
Te Tiratū is calling on the Crown to ensure the implementation of 12-month prescriptions strengthens rather than weakens safety and equity, including through:
• Mandatory, equity-focused monitoring, with prescribing rates disaggregated by ethnicity, rurality, deprivation, disability, and continuity of care
• Transparent reporting of adverse events, hospitalisations, medicine changes, and wastage
• Māori-led evaluation of safety, trust, communication, and cultural safety
• Clear national guidance on who is not clinically appropriate for 12-month prescriptions
• A Te Tiriti-aligned medicines optimisation strategy, grounded in Pae Ora and mātauranga Māori
“Extending prescription duration alone will not improve health outcomes for Māori,” says Brandi Hudson.
“For a small number of whānau, longer prescriptions may be appropriate but only within a broader, equity-led system of care. Without strong safeguards, this policy risks entrenching, rather than reducing, inequity.”

Policy changes to prescription medicines must not place Māori at higher risk of harm or delayed care.
How this change to prescription medicine impacts our whānau from Tainui waka rohe.
Position Statement – 12-Month Prescriptions

Te Tirātū Iwi Māori Partnership Board believes that extending prescriptions to 12 months, without strong safeguards, risks deepening medicines-related inequities for Māori. While longer prescriptions may benefit a small number of clinically stable patients, Māori already face under-diagnosis, reduced monitoring, fragmented care, and culturally unsafe prescribing. Prescription duration alone cannot address barriers such as cost, transport, limited continuity of care, and systemic bias, and may increase under-care, delayed treatment, and medicine-related harm.
Te Tirātū calls on the Crown to implement 12-month prescriptions only within a Te Tiriti-aligned, equity-led framework. This must include mandatory monitoring of access and clinical safety, Māori-led evaluation, culturally safe practice, clear standards for review and prescribing, and formal recognition of rongoā Māori. Without these measures, long-duration prescriptions risk entrenching inequities rather than improving the safety, mana, and wellbeing of whānau Māori.
References:
[1] Te Karu, L. (2021). Restoration of the health system must not neglect medicines – but who has the power of reform? Journal of Primary Health Care, 13(2), 96–101.
[2] Te Karu, L , Bryant, L., Harwood, M., & Arroll, B. (2018). Achieving health equity in Aotearoa New Zealand: The contribution of medicines optimisation. Journal of Primary Health Care, 10(1), 11–15.
[3] Horsburgh, S., & Norris, P. (2013). Ethnicity and access to prescription medicines. The New Zealand Medical Journal, 126(1384), 7–11.
[4] Metcalfe, S., Beyene, K., Urlich, J., Jones, R., Proffitt, C., Harrison, J., & Andrews, Ā. (2018). Te Wero tonu-the challenge continues: Māori access to medicines 2006/072012/13 update. The New Zealand Medical Journal, 131(1485), 27–47.
[5] Waitangi Tribunal. (2019). Hauora. Report on Stage One of the Health Services and Outcomes Kaupapa Inquiry. WAI 2575. Waitangi Tribunal Report 2019. Waitangi Tribunal. https://www.waitangitribunal.govt.nz/news/report-on-stage-one-of-healthservices-and-outcomes-released/
Policy changes to prescription medicines must not place Māori at higher risk of harm or delayed care.
How this change to prescription medicine impacts our whānau from Tainui waka rohe.
Te Tiratū Iwi Māori Partnership Board member named new chair
Our Board member and clinician, Dr Mataroria Lyndon (MBChB, MPH, PhD), is the newly appointed Chair of the Whānau Ora Investment Board for the Upper North Island. He speaks to Waatea about the Board’s vital role in directing government resources to support whānau wellbeing. Under her leadership, the Board will continue to champion locally driven, culturally aligned initiatives that deliver sustainable, long-term outcomes for whānau across Aotearoa.
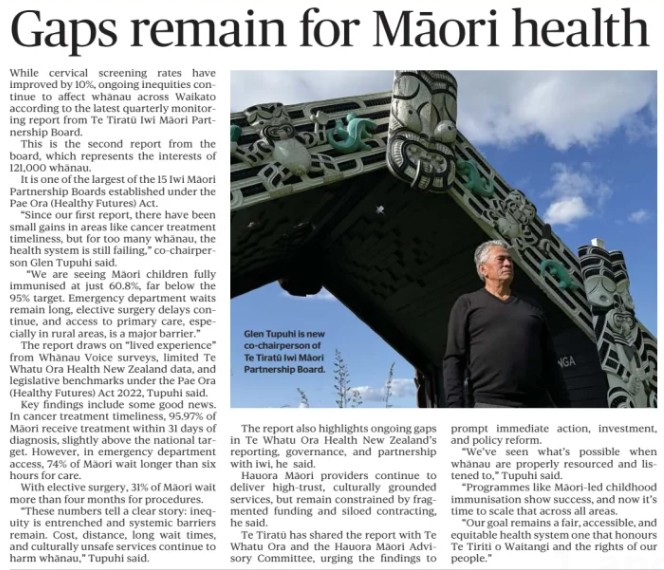
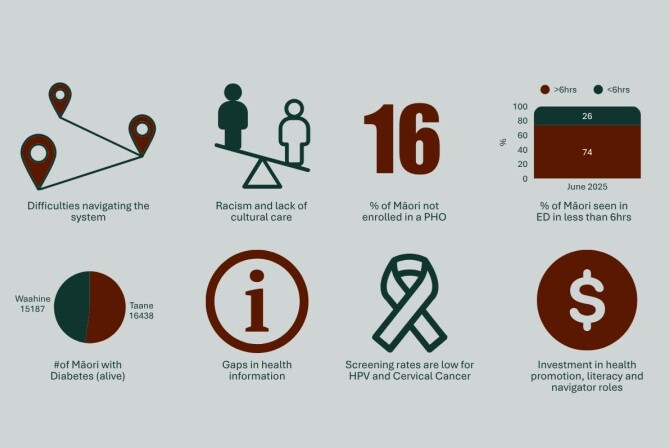
Gaps remain in Māori health
The Waikato Local has covered Te Tiratū Iwi Māori Partnership Board’s latest Quarterly Monitoring Report on the health system, which highlights persistent health inequities for Māori across the Tainui waka rohe. While small gains were seen in cervical screening and timely cancer treatment, major gaps remain: only 60.8% of Māori children are fully immunised at 24 months, long emergency department waits affect 74% of Māori, and nearly a third face elective surgery delays over four months. Co-Chair Glen Tupuhi calls for immediate action, investment, and scaling of Māori-led health initiatives.
New chair of Whānau Ora investment board across Upper North Island

From left to right (Front): Ernestine Walsh, (Chair) Dr Mataroria Lyndon, Riana Manuel, (Back) Leon Wijohn, (CE) Te Rōpu Poa, Dr Leanne Te Karu.
Te Tiratū Iwi Māori Partnership Board warmly congratulates Dr Mataroria Lyndon, on his appointment as Chair of the Rangitāmiro Whānau Ora Commissioning Agency Investment Board in a region of 2.3 million across the upper North Island.
“Rangitāmōro reflects the collective strength and vision of Te Tiratū Iwi Māori Partnership Board, Ngā Pou Hauora o Tāmaki Makaurau, and the National Hauora Coalition (NHC) who are tripartite partners,” said Glen Tupuhi, co-chair of Te Tiratū Iwi Māori Partnership Board.
“The leadership under Mataroria alongside that of his fellow board members gives us confidence that Rangitāmiro will advance what matters most to our people. The oranga and mana motuhake of whānau living in Te Tai Tokerau to Tūwharetoa, including Tāmaki Makaurau, Waikato and Hauraki.”
This critical leadership role places Dr Lyndon at the centre of strategic investment and assurance for Whānau Ora commissioning in the largest Whānau Ora region of Aotearoa.
Rangitāmiro is one of four newly contracted agencies operating under the Government’s Whānau Ora commissioning model.
The Investment Board is a structural safeguard to provide independent investment advice on how to best distribute funding to meet regional need. It will provide data‑informed direction on priorities, needs analysis, workforce planning and allocative frameworks all designed to strengthen confidence in investment decisions and outcomes.
“What makes this Board particularly significant is the breadth of expertise it brings from across whānau wellbeing, economic development, Hauora, social investment, commercial governance and Mātauranga Māori,” Dr Lyndon said.
“We will provide advice that directly informs commissioning priorities, regional needs analysis and workforce planning – key inputs for disciplined, evidence‑grounded decision‑making.”
The Investment Board’s membership reflects deep regional representation and technical expertise, and includes:
- Dr Mataroria Lyndon, Chairperson (Ngāti Hine, Ngāti Wai, Ngāti Whātua, Waikato‑Tainui)
- Riana Manuel (Ngāti Pūkenga, Ngāti Maru, Ngāti Kahungunu, Ngāti Whanaunga)
- Leon Wijohn (Ngāpuhi, Te Rarawa, Ngāi Tūhoe, Ngāti Tahu‑Ngāti Whaoa)
- Dr Tristram Ingham, KSO, MNZM (Ngāti Kahungunu, Ngāti Porou)
- Ernestynne Walsh (Ngāti Porou,Te Whānau‑a‑Apanui)
- Dr Leanne Te Karu (Ngāti Rangi, Te Ati Haunui-a-Pāpārangi, Muaūpoko)
The Investment Board sets investment priorities that are informed by whānau aspirations and evidence and guides allocative frameworks across the region to maximise both impact and equit
The Board provides strategic advice on a wide range of planning and investment activities, including the three-year Regional Needs Analysis, Investment Plans, and Regional Workforce Plans, while monitoring impact and performance to ensure that public investment delivers real value for whānau and communities.
Rangitāmōro has already contracted 301 kaimahi, including 120 new roles, to meet growing needs across its rohe from Tuwharetoa to the Far North, supported by a Government‑signalled Whānau Ora funding envelope of up to NZ$66,552,000 million per year for region 1 in 2025/26 and beyond.
Dr Lyndon brings significant governance and commercial experience to the role across health, research and governance sectors. He serves on multiple boards, including Rangitāmiro, and Te Tira Tū Iwi Māori Partnership Board, co-founding Tend Health, lecturing at the University of Auckland, and advocating for cultural safety to improve health outcomes, holding degrees from Harvard and Auckland.
His leadership underscores the commitment of Rangitāmiro to rigorous investment planning and assurance processes, in line with TPK’s commissioning model and expectations of arm’s‑length independence.
Some gains, many gaps remain for Māori health - System monitoring report
MEDIA STATEMENT
FOR IMMEDIATE RELEASE
Wednesday 3 December 2025, 9:00 AM
2 minutes to Read
Te Tiratū Iwi Māori Partnership Board has released its latest Quarterly Monitoring Report, the second this year reviewing health system performance across the Tainui waka rohe in Waikato.
It builds on its inaugural report from June 2025 representing the interests of 121,000 whānau. While cervical screening rates have improved by 10%, ongoing inequities continue to affect whānau across the rohe.
“Since our first report, there have been small gains in areas like cancer treatment timeliness, but for too many whānau, the health system is still failing,” says Co-Chair Glen Tupuhi of one of the largest of the 15 Iwi Māori Partnership Boards established under the Pae Ora (Healthy Futures) Act.
“We are seeing Māori children fully immunised at just 60.8% far below the 95% target. Emergency department waits remain long, elective surgery delays continue, and access to primary care, especially in rural areas, is a major barrier.”
The report draws on lived experience from Whānau Voice surveys, limited Te Whatu Ora Health New Zealand data, and legislative benchmarks under the Pae Ora (Healthy Futures) Act 2022. Key findings include:
• Cancer treatment timeliness: 95.97% of Māori receive treatment within 31 days of diagnosis, slightly above the national target.
• Elective surgery: 31% of Māori wait more than four months for procedures.
“These numbers tell a clear story: inequity is entrenched and systemic barriers remain. Cost, distance, long wait times, and culturally unsafe services continue to harm whānau,” Tupuhi says.
The report also highlights ongoing gaps in Te Whatu Ora Health New Zealand’s reporting, governance, and partnership with iwi. Hauora Māori providers continue to deliver high-trust, culturally grounded services, but remain constrained by fragmented funding and siloed contracting.
Te Tiratū has shared the report with Te Whatu Ora and the Hauora Māori Advisory Committee, urging the findings to inform immediate action, investment, and policy reform.
“We’ve seen what’s possible when whānau are properly resourced and listened to,” Tupuhi says.
“Programs like Māori-led childhood immunisation show success, and now it’s time to scale that across all areas. Our goal remains a fair, accessible, and equitable health system one that honours Te Tiriti o Waitangi and the rights of our people.”
Background
Locality of Te Tiratū Iwi Māori Partnership Board represents the local Māori voice from:
1. Waikato – Central North Island, extending from the west coast (Raglan) inland to Hamilton and south towards Taupō.
2. Hauraki – Northern Waikato and the Coromandel Peninsula, bordering the Firth of Thames.
3. Maniapoto – Western-central North Island, covering the King Country, including Te Kūiti and Ōtorohanga.
4. Raukawa – South Waikato and central North Island, including Tokoroa, Putāruru, and Tirau.
5. Ngāti Hāua – Western-central North Island, around Taumarunui and the western Ruapehu district.