Rural Health Roadshow: Te Kūiti Speaks
Yesterday, the Les Munro Centre in Te Kūiti was packed as Te Tiratū Iwi Māori Partnership Board attended the Rural Roadshow. Mental Health Minister Matt Doocey and Minister for Rural Communities Mark Patterson listened as the community spoke directly about the real issues affecting them so both ministers and bureaucrats heard their voices firsthand.
Minister Doocey admitted that while national targets for health services may appear strong, performance in rural areas, particularly for rangatahi Māori mental health, lags significantly behind.
“Nationally we might be hitting 80 percent, but in rural Māori communities, the figures drop sharply,” he said. He praised the importance of local decision-making, stressing that community knowledge is essential to design effective services, and shared that the government is prioritising investment in underperforming areas, with $2.8 billion committed to mental health services this year, aiming to resource local providers and lift access and outcomes.
Key Questions from the Community
Local doctors, Kaimahi, and hauora Māori providers raised concerns that included access to care, noting that in some rural areas travel times to a hospital can exceed three hours, meaning urgent care is often delayed. Workforce shortages were another pressing issue, with providers asking what strategies will be implemented to retain doctors, nurses, and Māori health practitioners in rural areas. Digital health limitations also surfaced, with communities highlighting the challenges of telehealth in areas without reliable internet. Sustainable funding and integration of services were other priorities, with providers questioning why many community services still receive only one-year contracts and how mental health, primary care, social services, and housing can be coordinated locally.
Various locals raised the broader determinants of health, including alcohol accessibility, youth vaping, housing, and poverty, noting that these factors directly influence mental health outcomes. A story was shared about intergenerational trauma, the lingering impact of war, and how past experiences of discrimination and stigma continue to shape the mental health landscape for whanau living rurally and remotely in the rohe today.
Ministers’ Responses
Minister Doocey spoke about targeted investment to underperforming regions and the importance of enabling local providers to design solutions from the ground up. Relational commissioning was highlighted as a key approach, allowing communities to develop services that meet their own needs rather than relying solely on top-down directives. He spoke about ambitious mental health targets, including one-week access for primary mental health services and three-week access for specialist services, among the fastest internationally.
Ministers discussed workforce development as a critical piece of the solution, encouraging rural students to pursue healthcare careers and return to their communities. Initiatives such as mobile health screening units, and integrated care prototypes currently on the drawing board as innovative ways to improve equity and access. Ministers also recognised the importance of preventative and early intervention services, stressing that timely support is vital to prevent minor health issues from escalating into serious conditions.
The meeting underlined that improving rural health requires both cross-agency government support and local leadership.
“Health isn’t just about seeing a doctor. It’s about housing, food security, education, and the broader environment. The government can pull a few levers, but ultimately communities drive what works,” said Minister Doocey.
Glen Tupuhi appointed to Te Tiratū role
The National Business Review (NBR) reports that Glen Tupuhi has been named co-chair of Te Tiratū Iwi Māori Partnership Board, joining Tipa Mahuta and succeeding Hagen Tautari. Te Tiratū, one of 15 boards established under the Pae Ora Act, represents around 121,000 Māori whānau across the Tainui waka region and ensures Māori perspectives shape local health services.
Tupuhi brings over 30 years of experience in Māori development across health, education, and justice, with leadership roles at Oranga Tamariki, Health Waikato, Hauora Waikato, Corrections, and Te Rūnanga o Kirikiriroa. He also serves on multiple boards, including Winton Land, Te Korowai Hauora o Hauraki, and the Hauraki PHO, and has led key economic and development initiatives in North Waikato.
Affiliating with multiple iwi across Waikato and Tāmaki Makaurau, Tupuhi’s appointment underscores Te Tiratū’s commitment to strong, culturally informed governance. Co-chair Tipa Mahuta welcomed him, thanking Tautari for his service and expressing confidence in Tupuhi’s leadership.
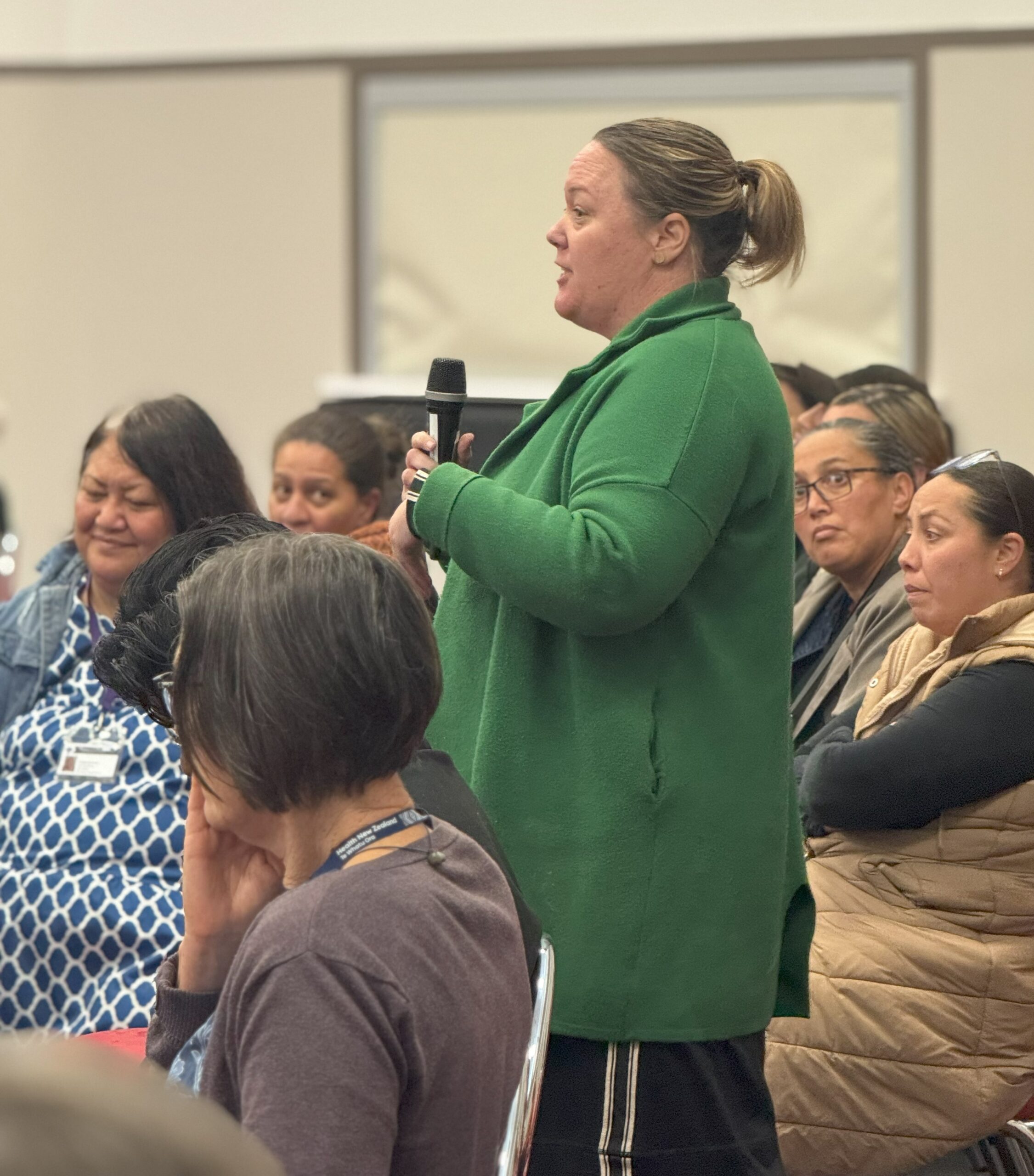
On the ground in Piopio: Health access struggles exposed at Te Nehenehenui Hui-ā-Tau

Photo: Whānau Voice kaimahi Raven Torea with kaumātua at Te Nehenehenui Hui-a-Tau
Whānau from Te Kūiti, Taumarunui, and surrounding areas came together at the Te Nehenehenui Hui-a-Tau, held at Napinapi Marae in Te Mapara, Piopio, to share their experiences with local health services, highlighting both the strengths of providers and the pressing gaps in care.
The hui, held on a clear and sunny day, provided an opportunity for kaumātua and whānau to discuss their needs and challenges with our Whānau Voice team. They reported using a mix of mainstream health services, including GP clinics, hospitals, dentists, midwives, physiotherapists, and optometrists, alongside traditional rongoā practices such as kawakawa teas, mirimiri, and herbal remedies. For many, GPs are a last resort, accessed only when traditional methods are insufficient.
Despite these resources, whānau emphasised the need for expanded services. Requests for more GPs, dentists, Māori-led health providers, mental health and counselling support, dieticians, and specialist services were consistent. Many whānau continue to travel to Waikato for care, often relying on friends or shuttles for transport, adding additional strain for elderly community members.
Access challenges were a recurring theme. Long wait times for GP and specialist appointments, lack of after-hours care, high costs for dental and optometry services, and limited information about available services all create barriers. Some whānau reported preferring to travel to Hamilton for glasses or dental care due to affordability and better service, highlighting inequities in local provision.
Despite these challenges, trusted providers received strong praise. Dr Rose Harris of the Maniapoto Whānau Ora Centre, which is part of the Taumarunui Community Kokiri Trust in Te Kūiti was highlighted as a Hauora Māori provider who delivers exceptional care, earning widespread respect from the community.
When asked about government health targets, whānau were unanimous in their assessment: the targets are not being met. “The government don’t see the struggles whānau have on the ground. They should walk in our shoes,” one wahine said. Another noted the higher rates of diabetes among Māori and Pasifika, adding, “No way. They’re not meeting them, and they need to go.”
Whānau also shared what supports their wellbeing. Engagement in marae and iwi activities, speaking te reo Māori, participating in physical activity, and spending time in nature were identified as key to maintaining health.
The hui underscored the importance of whānau voices in shaping health services. Whānau called for care that is accessible, culturally grounded, and delivered by Māori providers close to home. Their message was clear: health systems must meet the needs of the people they serve.
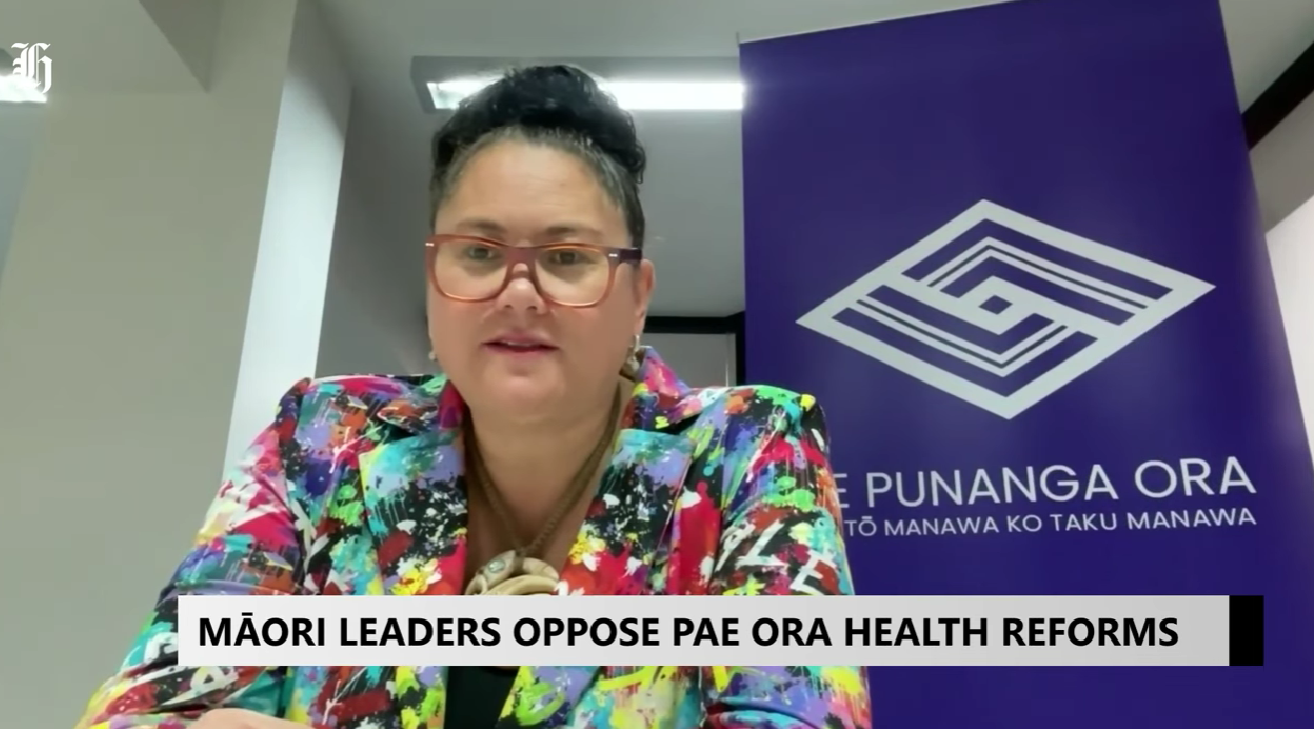
Iwi Māori Partnership Boards concerned their role minimised under Pae Ora Act changes
Photo: Te Manawa Taki IMPB collective member, Te Taura Ora o Waiariki Chair Hingatu Thompson
RNZ reports about the unified stance of all 15 Iwi Māori Partnership Boards (IMPBs) coming together in Taranaki for a two-day National Hui, expressing concern that proposed changes to the Pae Ora (Healthy Futures) Act would diminish their role in New Zealand’s health system. Te Tiratū Iwi Māori Partnership Board shares this opposition, highlighting that local, iwi-led decision-making and accountability are essential to improving Māori health outcomes.
Leaders at the hui said that the proposed amendments risk silencing Māori voices, removing direct iwi oversight, and limiting the ability to deliver whānau-centred health solutions. IMPBs were established under Te Tiriti o Waitangi principles to ensure Māori engagement with the Crown, guide local health strategies, and address systemic inequities such as lower life expectancy and poorer outcomes for Māori.
The hui highlighted concerns over four key areas: maintaining Te Tiriti protections in legislation, ensuring the Hauora Māori Advisory Committee is accountable to iwi, retaining a Māori health strategy, and preserving the critical role of IMPBs in regional health planning. Te Tiratū reinforced that strong local partnerships and culturally responsive approaches are vital to achieving equity and improving Māori health.
Iwi Māori partnership boards unite to oppose changes to health legislation
Photo: Te Tiratū Iwi Māori Partnership Board Co-chair Hagen Tautari
Iwi Māori Partnership Boards (IMPBs) from across Aotearoa are standing together to oppose proposed amendments to the Pae Ora Act, raising concerns that the changes would weaken their statutory role and reduce Māori oversight in the health system. The fifteen boards, representing over 900,000 Māori, are meeting in New Plymouth for the first time since the Bill’s first reading to build a unified national voice, safeguard local accountability, and ensure health services remain responsive to whānau needs. The hui and the boards’ stance have been covered by 1News/Te Karere highlighting the nationwide concern that these changes could undermine decades of partnership work and progress in Māori health equity.
Iwi Māori partnership boards unite to oppose changes to health legislation
The stance of Te Tiratū as part of a national alliance of 15 IMPBs united in opposition to proposed amendments to the Pae Ora (Healthy Futures) Act has been covered by Te Karere, highlighting the national conversation around Māori leadership in health.
The national collective warns that the changes would weaken Te Tiriti-based partnerships and threaten Māori health equity. The National IMPB Hui in New Plymouth attracted representatives from 82 iwi, representing the interests of over 900,000 Māori. Rangatahi attendees highlighted the links between hauora, whakapapa, and whenua, reinforcing the need for health solutions that integrate ancestral knowledge with modern systems.
A Te Tiratū spokesperson emphasised that IMPBs must remain active partners in shaping local and regional health strategies, including targeted Māori equity actions, and that any amendments undermining Te Tiriti principles must be opposed.
Our nationwide stand with all IMPBs against proposed Pae Ora Bill changes

Photo: Board member Maxine Ketu and e Tiratū Tumu Whakarae, Brandi Hudson attend the National IMPB Hui in New Plymouth
Te Tiratū Iwi Māori Partnership Board (IMPB), as part of a national alliance of 15 IMPBs, opposes the proposed amendments to the Pae Ora Act, warning that the changes would weaken Te Tiriti-based partnerships and undermine progress in Māori health equity.
At a recent National IMPB Hui in New Plymouth, 15 IMPBs representing 914,400 Māori from 82 iwi aligned in opposition to the Bill. The discussions highlighted the critical importance of maintaining partnerships that are rooted in trust, respect, and intergenerational thinking, ensuring solutions are anchored in mātauranga Māori and the realities of whānau.
The hui included rangatahi voices emphasising the deep connections between hauora, whakapapa, and whenua. Their presentations stressed the need for health approaches that integrate ancestral knowledge with modern, data-driven health systems. This interweaving of the old and the new highlighted the value of locally led solutions that resonate with whānau and communities.
Te Tiratū IMPB asserts that the proposed changes would remove direct iwi accountability, replacing kanohi ki te kanohi relationships with a centralised, Minister-appointed process. This approach risks tokenistic consultation rather than genuine Māori leadership, and threatens the hard-won equity gains achieved by IMPBs over the past decade.
The Board’s position is clear: local accountability through IMPBs must remain, regional advice to Te Whatu Ora must be strengthened, and health strategies must include specific Māori equity actions. Any amendments that weaken or replace Te Tiriti principles are opposed.
Te Tiratū IMPB submitted its formal response to the Health Committee on 18 August 2025, supporting a unified IMPB call to:
- Retain HMAC accountability to iwi through IMPBs
- Strengthen IMPB roles for local and regional advice to Te Whatu Ora
- Develop health strategies with targeted Māori equity actions
- Oppose amendments that undermine Te Tiriti principles
Our Board emphasises that this is about safeguarding the right to lead local solutions for Māori communities. Analysis shows the proposed changes are unlikely to improve Māori health outcomes, reinforcing the need to maintain systems that are already showing results.
Te Tiratū IMPB remains committed to advocating for whānau-centred health solutions and ensuring Māori voices remain central in shaping Aotearoa’s health system.
Māori leaders oppose Pae Ora health reforms
Photo: Te Manawa Taki IMPB collective member, Tūwharetoa Iwi Māori Partnership Board Chair Louisa Wall at the National IMPB hui
All 15 Iwi Māori Partnership Boards (IMPBs) gathered in Taranaki to oppose proposed amendments to the Pae Ora (Healthy Futures) Act, warning the changes would significantly reduce their role, including removing critical monitoring powers. Louisa Wall, Chair of Tūwharetoa Toa IMPB, when interviewed by HeraldNOW, explained that IMPBs were created following the Waitangi Tribunal’s 2019 recommendation and the Simpson Review to address systemic inequities, including institutional racism, and to ensure Māori voices shape health services.
Wall said that Māori often access healthcare too late, and IMPBs are uniquely positioned to support preventative initiatives, immunizations, and screenings through a Māori, rural, disability, and patient-centered lens. She criticized the government’s move to shift authority to the Minister-appointed Hauora Māori Advisory Committee, saying it cuts iwi and hapū out of decision-making and undermines the partnerships that are essential for transforming the health system and improving equity for all New Zealanders.
What whaanau told us at Tainui Hui-aa-Tau

Photo: Whaaea Audrey Wildermott, Ngaati Koroki Kahukura with Whaanau Voice kaimahi
Te Tiratū Iwi Māori Partnership Board was honoured to attend Tainui Hui-aa-Tau 2025, hosted by Tainui iwi walking in the steps of their visionary Koiora strategy. This aspirational kaupapa brought together thousands of uri and providers across the motu to connect, share, and strengthen collective oranga.
We were there by invitation to support Whaanau Voice and deepen our understanding of how the Koiora Collective and Te Tiratū fit within the wider ecosystem of Māori health and wellbeing. While our original focus was on promoting our Oranga Survey the day quickly turned into something more — a space for heartfelt koorero and deep listening.
What we heard was despite government targets focused on faster cancer treatment, shorter ED stays, improved immunisation, and reduced wait times for specialist and elective care, whaanau at Tainui Hu-a-Tau described a system that remains slow, hard to access, is culturally disconnected, and difficult to navigate — especially for whaanau seeking kaupapa Maaori services and timely, affordable care.
Whaanau Voice Leads the Way
Our space at Hui-aa-Tau was a hive of activity, filled with whānau keen to share their experiences and insights about accessing healthcare. Many whaanau wanted to koorero at length, reflecting a widespread desire to be heard. Primary care was a consistent topic. Whānau spoke about long GP wait times, often up to four weeks, difficulty enrolling at kaupapa Maaori clinics due to capped rolls, and the frustration of not being able to see the same doctor for continuity of care. Many whaanau living rurally shared feelings of isolation from healthcare, relying on transport support from whaanau, iwi or local services. For those who could afford it, urgent care was preferred over long waits at emergency departments, but even this came with financial strain.
The Strain of Financial Pressure
Cost was a major barrier. Whaanau shared stories of having to choose between kai and seeing a doctor. Prescriptions added another burden. Even if a whaanau member managed to secure an appointment, the costs didn’t end there. Some spoke of giving up altogether — delaying care or avoiding it until it became urgent. Many whaanau weren’t enrolled with a GP at all. Some had been trying to enrol with kaupapa Maaori services but were turned away due to capacity limits. Several questioned why non-Maaori were enrolled in Maaori-specific services when they, as tangata whenua, were being declined. There was deep mamae in these koorero, and a desire for a fairer, more culturally grounded system.
The Challenge of Health Literacy for Kaumatua
Kaumatua shared personal journeys of navigating health conditions and the system without proper explanations or support. One kaumatua described an 18-month journey to get assistance to help manage his diabetes to get it under control which is a long time to be mauiui. Others expressed confusion around medication or what services were available to them. Many didn’t know where to go or how to ask for help, and several mentioned feeling whakamaa about not understanding their conditions. The language barrier was another big one, where whaanau are not able to understand a lot of different accents by non-Maaori health practitioners, they feel there is a lack of cultural safety too. For kaumatua living rurally, transport remains another major barrier. Many said that it was much easier for them to go to their local marae that was close. Many rely on once-a-week iwi transport or local hauora hubs that have now been scaled back due to funding cuts. In some areas, services that once operated five days a week now open for just one — creating high demand and limiting access.
Mental Health in Crisis
Mental health was another area of concern. Many who spoke were supporting a sibling, cousin or other whaanau member. The main issue raised was the lack of support available before a person reaches crisis or hospitalisation. Henry Bennett Centre came up repeatedly — described as difficult to deal with, lacking cultural safety, and disconnected from whaanau. Whaanau described not being informed about loved ones’ care, feeling shut out of the process, and being left to advocate for their whaanau without support.
There was a strong call for mental health services that are proactive, culturally safe, and easy to navigate. Many felt stuck trying to get help for their whaanau and repeatedly faced barriers in the process.
The Hidden Gaps in Women’s Health
A number of wahine raised concerns about the lack of accessible information around menopause. They described debilitating symptoms and feeling unsupported or dismissed. Some were surprised to learn just how little was publicly available in terms of education and care. The koorero made it clear that more kaupapa Maaori women’s health services are needed — both in delivery and in design.
Hearing Loss, Delayed Care and Advocacy
Hearing support was another unexpected but prominent theme. Many whaanau attending the hui wore hearing aids, yet no hearing-focused service was present. One kaumatua, a veteran of the New Zealand Army, shared that it took years to realise the extent of his hearing loss. Another wahine described the two-year process of trying to get care for her daughter — eventually only made possible with the help of a Maaori advocate. For these whaanau, accessing support required determination, energy, and navigating complex systems. Funding options, eligibility, and appointment access created further layers of stress. Even for tamariki, care was delayed — sometimes for years. While support grants like the kaumatua hearing aid fund exist, awareness and accessibility remain major gaps.
The Need for Rongoaa and Kaupapa Maaori Options
Throughout the day, whaanau called for more access to mirimiri and rongoaa Maaori. There was a hunger for services that reflect maatauranga Māori and are grounded in whakapapa and whaanau values. One whaanau member, supporting a younger relative who had experienced a stroke, spoke of the lack of Maaori-led recovery options. Others expressed interest in alternatives to mainstream medication but didn’t know where to start. The desire for Maaori-led, whaanau-centric, culturally affirming care was one of the strongest themes to emerge. It aligns closely with the aspirations of Tainui’s Koiora strategy and the values Te Tiratū holds as we walk alongside whaanau and providers.
A Call to Honour Whaanau Voice in System Change
Tainui Hu-aa-Tau 2025 was more than an event — it was a collective pulse check on how the health system is serving our people. Whaanau were open, honest, and generous with their koorero. Their insights paint a clear picture of a system that needs to evolve, one that genuinely centres Whaanau Voice, upholds Te Tiriti o Waitangi, and recognises hauora as a right, not a privilege. We are committed to carrying these voices forward — into our planning, our advocacy, and our partnership with Te Whatu Ora. We also mihi to Tainui iwi for their bold leadership and vision, and for the opportunity to stand together in kaupapa Maaori-led transformation. Te Tiratū will continue to listen and act — because when whaanau speak, the system must listen and respond.
"Kāore e taea te whakamāhara i tēnei wā” – Kura rata hou ki Waikato
Kua whakaaetia e te kāwanatanga he pūtea mō tētahi kura rata hōu ki Te Whare Wānanga o Waikato, ka whakatūria hai te tau 2028.
Ka whakangungua e tēnei kura ngā rata hōu mō ngā hapori tuawhenua me ngā rohe kāore i te pātata ki ngā ratonga hauora.
Hai tā te Tiamana takirua i te Poari o Te Tiratu, e ai ki a Hagen Tautari, ko te mahi mā Te Tiratu ki te kura rata ko te whakatō i ngā wāriu Māori hai pae ārahi i ngā whakahaerenga katoa, mā reira e ū ai te kura ki ngā mātāpono o te ao Māori.