What’s really happening with cancer screening our rohe

Cancer impacts countless whānau across Waikato—and feedback from 23 whānau within the Tainui waka region, together with broader insights from our Community Health Plan, initial Monitoring Report, and engagement efforts from March to June, is revealing what’s effective, what’s falling short, and where services need to improve.
Our first Monitoring Report, released this month, shows that breast screening rates for wāhine Māori in Waikato continue to lag behind. Currently, just 54.5% of our wāhine are up to date with screening—7% lower than the national rate for non-Māori (64.6%). While there has been a small improvement of 1.1% since the last quarter, the pace of change remains too slow to close the equity gap.[1]
Most surveyed by our Whānau Voice team (nearly 74%) told us they regularly take part in cancer screening, particularly breast and cervical checks. Many said this is driven by personal or whānau experience of cancer. One participant shared: “My mum had cancer… I made self-referrals. I know how important it is to catch it early.”
But behind those statistics lies a more complex picture. Screening isn’t always comfortable. Over half of respondents said the process left them feeling whakamā, exposed, or in pain. Several described experiences that were rushed or poorly explained—leaving them uncertain, anxious, or unlikely to return. One woman shared: “Didn’t want to go back after last time—felt exposed.” Another added: “It was painful and no one explained anything.”
This discomfort was often made worse by a lack of cultural safety. Māori participants talked about mispronounced names, feeling spoken over, or being asked sensitive questions without privacy. “The lady at reception was white and made no effort to pronounce my Māori name,” said one. Others spoke of rushed appointments and the feeling that their experience wasn’t respected or mana-enhancing.
Not everyone receives timely results, either. Some whānau said they had to chase clinics for updates, while others described waiting months for treatment—even when a diagnosis had already been made. One respondent noted: “We waited 3–4 months, even with private insurance. Treatment took 6–9 months. Too long.”
The good news? Whānau know what would help.
They asked for more Māori doctors and support workers, better access to information, and culturally grounded care that includes warm, respectful service and more whānau-friendly settings—like marae, mobile clinics, or iwi spaces. Many called for free screening for kaumātua, flexible appointment times, and reminders by text or email, noting that these are not offered consistently.
Suggestions were practical and clear:
- “More Māori health professionals, please.”
- “Better-informed and pre-screening promotion.”
- “Use marae and iwi groups to get the message out.”
- “Have a Māori support person due to the medical language.”
A little over half of those surveyed also had a whānau member diagnosed with cancer in the last three years, and nearly half of them said they did not receive enough information about the treatment journey or support services.
There’s a clear call here—not just for more education and outreach, but for services that genuinely listen, respond, and hold space for whānau with care. As one whānau put it: “We need more manaaki-focused care. It makes all the difference.”
This kōrero reinforces the need for screening services that don’t just invite people in but hold them with dignity, understanding, and culturally safe support. Because early detection saves lives—but only if our people feel safe enough to walk through the door.
[1] Pg 13 Source: https://tetiratu.co.nz/wp-content/uploads/2025/07/2025-Te-Tiratu-IMPB-Monitoring-Report-to-March-2025.pdf
GP door closed for many: Whānau speak out

Photo: Kuia providing feedback at a recent Taumarunui Hapori Hauora Day
“We waited eight hours, and no one even told us how long it would be.”
This is the reality for many Māori whānau in the Waikato region, as shown in the latest Whānau Voice quarterly results that reveals the deep cracks in our primary care system.
These insights are drawn from a snapshot survey completed by 88 participants, alongside wider data gathered through our Community Health Plan, first Monitoring Report and engagement activities held between March and June. Their voices paint a clear picture judging by the indicative results, that our local health system is under immense pressure, and it’s pushing whānau to breaking point.
Despite more than 90% of respondents being enrolled with a regular GP, nearly 40% said they were unable to get an urgent appointment when they needed one. For many, the GP door feels effectively closed—whether due to fully booked clinics, high costs, or services being unavailable altogether.
In the first Health System Monitoring Report by Te Tiratū released this month, we note that key data from Te Whatu Ora is still missing. This includes:
- GP enrolment figures compared to the population (Māori vs non-Māori by age)
- Māori utilisation of GP services over the past 12, 24, and 36 months
- Māori utilisation by type of service (in-clinic vs virtual)
This lack of data limits our ability to assess equity in access and use of primary care services for Māori.[1]
So, in these moments of urgency, whānau are being forced to turn to urgent care clinics or hospital emergency departments for care that should be delivered by a GP. Nearly three-quarters of those surveyed said they had gone to A&E when they couldn’t get a GP appointment.
Of those, 29 percent reported waiting six to eight hours. Nine percent said they waited more than ten hours. Most waited without receiving any updates or basic information—86 percent received no health information during their wait, and 84 percent weren’t told how long the wait would be.
Adding to the strain, more than half of respondents said cost had stopped them or their whānau from getting care. This was particularly true for those in remote or rural areas like Tokoroa, Waharoa, and Huntly, where choices are limited and even getting to a clinic can be a challenge.
Some whānau reported being unable to enrol with a GP because no clinics were accepting new patients, or they lacked the required ID. These are not isolated stories; they reflect systemic barriers that need urgent attention.
What is Working?
Not all findings were bleak. Most people reported being able to get planned appointments when needed, and those who used telehealth services found them useful—90 percent said the advice met their needs.
Enrolment in a regular general practice remains high, which shows that there is a foundation to build from. But trust and consistency remain issues, with more than half saying they don’t get to see the same doctor each time.
This survey doesn’t just reveal long wait times or stretched services—it highlights the emotional weight of a system that too often leaves Māori whānau out of reach. It tells a story of people navigating closed doors, cost barriers, and uncertainty, just to access the care they deserve.
Te Tiratū Iwi Māori Partnership Board is using this data to advocate for urgent investment in services that are responsive, affordable, and culturally safe. Because no one should have to wait ten hours in an emergency room for care that should have been delivered in a clinic—least of all our tamariki and kaumātua.
[1] Pg 4 Source: https://tetiratu.co.nz/wp-content/uploads/2025/07/2025-Te-Tiratu-IMPB-Monitoring-Report-to-March-2025.pdf
From knowing to showing: Social value in focus at provider Forum

Photo: Te Tiratū Tumu Whakarae, Brandi Hudson (right) with Christine Arihia Brears (second right) and her kaimahi who travelled all the way from Taumarunui Kokiri Trust and Maniapoto Whanau Ora Centre to the Forum.
How do we truly shift the dial on health outcomes for whānau? For Te Tiratū Iwi Māori Partnership Board, the answer lies in listening to our providers, communities, whānau, aligning systems, and proving impact.
On Friday, over 30 kaimahi gathered at the Waikato Innovation Centre for Te Tiratū’s second Provider Forum, where Tumu Whakarae Brandi Hudson shared an update on kaupapa milestones before the rōpū moved into a wānanga on how data—can be a powerful tool for transformation, including a deeper kōrero on Social Return on Investment (SROI).
Two self-confessed, “old hands at this” Tammy Lehar and Susan Turner appreciated how space was created for partners who haven’t yet had the opportunity or experience, to come into a common kōrero together. “It’s something beautiful — if it’s done with the right intentions,” they said.
Tammy also highlighted the importance of building intentional data infrastructure “so we’re collectively working towards a shared vision—rather than duplicating efforts or collecting data in siloes.”
“We have the National Iwi Board Chairs Forum and the Iwi Māori Partnership Boards (IMPBs) with a common intention of strengthening data collection in this space. But to create meaningful connections between data and whānau outcomes, we must first build strong, integrated connections between these existing and emerging infrastructures—especially if we’re committed to a Whānau Ora approach.”
“This requires multiple, layered conversations. Personally, I’d challenge the assumption that Primary Health Organisations (PHOs) alone can provide a full picture, as they mainly reflect the primary health care lens. We also need to draw on data from other sectors, such as those funded under MSD and elsewhere, to understand the broader context of whānau wellbeing,” she said.
“There’s a foundational conversation needed—both at a local level and across the larger infrastructure. These discussions are already happening, but it takes time to bring the right people together in the right forum.” Innovation analyst Mari Tanioka from ImpactLab shared case studies on how to turn deep community knowledge into visible, trusted evidence.
“It’s a shift from knowing your mahi matters, to showing it clearly—using stories, numbers, and whānau voices. Often, what’s seen as anecdotal or informal is actually powerful insight. When made visible, it becomes a force for accountability and change,” she said.
Mari encouraged providers to start simple—by collecting clear, useful data such as how many whānau are being reached, or what barriers they face.
She gave the example of a provider who discovered, by tweaking just one survey question, that they were reaching over 63,000 tamariki—far more than they had previously realised. That kind of insight validates the mahi of kaimahi and helps funders better understand the scale and impact of their work.
The forum brought the philosophy of social investment into sharp focus. In a world of scarcity, complexity, and urgency, targeted support can change the course of a life. The difference between what a whānau’s future might look like without help—and what becomes possible with it—is what we call social value.
“Transforming lives through targeted interventions”— that, said Mari and her colleague Sarah Tuck, Engagement Manager at ImpactLab, is the heart of social investment.
Measuring that difference isn’t just about proving value—it’s about understanding what really works. Mari shared how one provider used SROI analysis to demonstrate that their slower, trust-based approach to health visits wasn’t inefficient—it was essential. With that evidence, they secured further funding.
Another organisation shifted strategy entirely, moving from diabetes treatment to prevention, after data showed how early engagement with whānau could help avert long-term harm.
For Te Tiratū, this mahi is about building strong, integrated systems that transform the system itself. Data alone is not the goal—it’s the pathway to transformation.
The shift from knowing to showing is more than a technical process. It takes time, care, and connection—but it’s what builds the momentum to reshape outcomes for our whānau, now and for generations to come.
Te Tiratū at the table of Rangitāmiro operating from Tūwharetoa to Te Tai Tokerau

Photo: Te Tiratū Tumu Whakarae, Brandi Hudson with Te Tiratū and Rangitāmiro Board member, Dr Mataroria Lyndon
Rangitāmiro is now fully operational, prepared to serve whānau across the largest region of all four new Whānau Ora Commissioning Agencies — stretching from the Far North to Tūwharetoa. This readiness is no accident. It reflects months of deliberate and intensive engagement, with more than 300 hui held with whānau and providers throughout Te Tai Tokerau, Tāmaki Makaurau, Waikato, Hauraki, and Tūwharetoa.
These conversations have shaped our approach and ensured that those already receiving Whānau Ora support will experience continuity, not disruption, during this transition.
Among those helping to lead this kaupapa is Dr Mataroria Lyndon (Ngāti Hine, Ngāti Wai, Ngāti Whātua, and Waikato) — a board member of both Te Tiratū Iwi Māori Partnership Board and Rangitāmiro. With deep whakapapa ties across the region and a lifetime of service to whānau health and Māori-led systems change, Dr Lyndon is confident that Rangitāmiro will continue to uplift whānau across Aotearoa.
From today, 301 Whānau Ora Navigators are on the ground through Rangitāmiro providers — reaching 100% of Rangitāmiro’s contracted target with Te Puni Kōkiri. This includes a net increase of 120 new kaimahi to meet the deep need across our rohe. These roles are not just numbers — they are trusted relationships, born from community, delivering support that reflects the real lives and aspirations of our whānau.
The Rangitāmiro commissioning model has also evolved. More pūtea will reach communities, where it is most needed. A stronger data system will help Rangitāmiro see what’s working, for whom, and why — improving outcomes and accountability. Direct relationships with providers will ensure transparency, responsiveness, and impact.
What remains unchanged is the unwavering focus of Rangitāmiro: whānau.
Whānau wellbeing. Whānau dreams. Whānau tino rangatiratanga.
A new dawn for whānau ora: Te Tiratū at the launch of Rangitāmiro
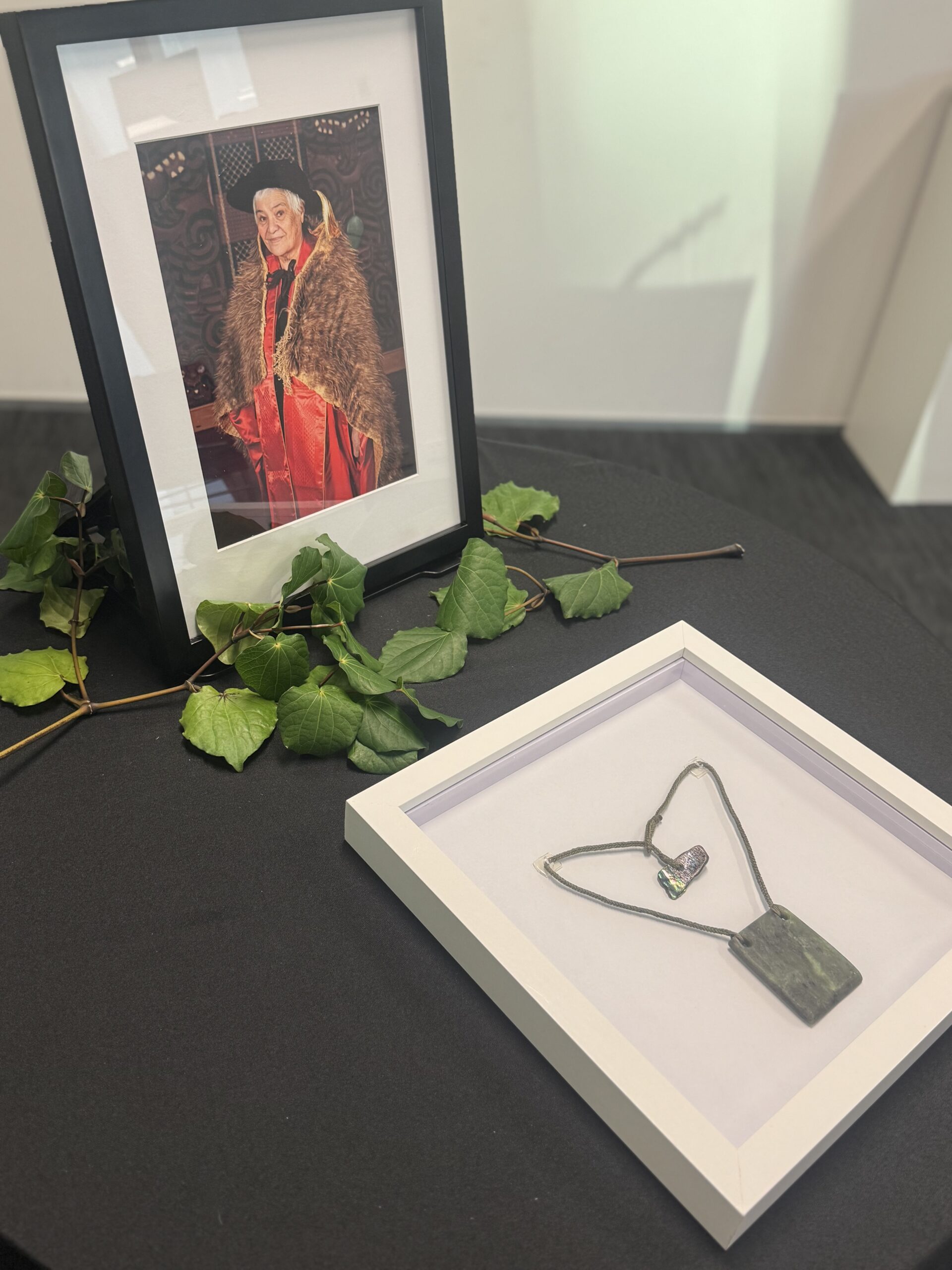
Photo: The late Kahurangi Tariana Turia and the mauri stone of Rangitāmiro
Early this morning, as the sun rose over Tāmaki, we gathered in karakia to mark the beginning of a powerful new chapter for Whānau Ora — Day One of Rangitāmiro, our new Whānau Ora Commissioning Agency for Te Tai Tokerau, Tāmaki Makaurau, Waikato, Hauraki and Tuwharetoa.
We carry forward the legacy of our beloved Kahurangi Dame Tariana Turia — with aroha, unity, and fierce determination. Her vision, rooted in manaakitanga, whanaungatanga, and tino rangatiratanga, continues to guide our mahi today. Whānau Ora is not just a policy; it’s a movement that centres whānau as the leaders and decision-makers of their own futures.
Rangitāmiro brings together the strength and vision of Te Tiratū Iwi Māori Partnership Board, Ngaa Pou Hauora oo Taamaki Makaurau, and the National Hauora Coalition (NHC). Together, we are focused on what matters most — the wellbeing and mana motuhake of our whānau.
Already operational, Rangitāmiro has contracted 301 kaimahi, including 120 new roles, to meet the growing needs of our region — from Tuwharetoa to the Far North. It holds the largest population of all four Commissioning Agencies and is committed to delivering services that support whānau across hauora, housing, kai security, oranga hinengaro, rongoā, financial wellbeing and more.
As a founding partner of Rangitāmiro, Te Tiratū stands proudly in our responsibility and honour to uphold Dame Tariana’s legacy. We were humbled to stand in karakia, to acknowledge our tūpuna, and to commit ourselves to this kaupapa once more — for our tamariki, our mokopuna, and all the generations to come.
“I mihi to all of the new commissioning agencies who put their hands up to continue this extraordinary mahi delivering Whānau Ora support. It’s evident that, despite it being our first day, it’s not our first experience with this kaupapa. We’ve been working with whānau for decades, and we’re resolute in taking those values, alongside the powerful legacy of Dame Tariana, forward into the future for our respective regions. Dame Tariana had always spoken of the importance of mahitahi, whanaungatanga, and manaakitanga for Whānau Ora,” Dr Mataroria Lyndon, Board member of both Te Tiratū Iwi Māori Partnership Board and Rangitāmiro.
Mā te huruhuru, ka rere te manu — with the right support, our people will soar.
Rangatahi real talk at the Kapa Haka regionals

Photo: Rangatahi with Ngatini Torea and Raven Torea, Whānau Voice kaimahi
“We’re aware. We just need more support.”
That was the clear message from rangatahi and whānau who engaged with our Whānau Voice kaimahi at the inaugural Te Mokotini ki Tainui and Tainui Secondary School Kapa Haka regionals over the weekend. Alongside thousands gathered to celebrate te ao Māori, haka excellence, and hāpori, our Te Tiratū stand was part of a ‘Hauora Hub’ inside the doors of Claudelands Event Centre. The whare was humming with conversation — and concern. From rangatahi to kaumātua, whānau shared openly about their health journeys, what’s working, and what’s failing them.
What Our Rangatahi Are Saying
Across two days, rangatahi spoke frankly about what they’re facing. They’re switched on and vocal about the lack of mental health and sexual health education in schools — especially around hauora hinengaro. Many shared they learn more from social media than from the classroom. They know mental distress is a problem among their peers but feel unsupported by the current system. They want more—more kōrero, more guidance, and more honest talk in safe spaces. One rangatahi said it best: “We talk about it on TikTok, but not in class. That’s not right.”
Vaping: From “Cool” to “Can’t Stop”
We were alarmed by how widespread vaping is among rangatahi, particularly those aged 12 to 17. Nearly all told us they had easy access — either through shops not checking ID or older siblings buying on their behalf. What began as something “cool” quickly became something they couldn’t stop. Many now feel addicted. They want to quit, but said it’s hard — and support is scarce.
Their message was clear: restrictions aren’t enough. They believe a total ban is the only way to truly protect rangatahi. Importantly, they also called for earlier education, aimed at tamariki aged 10–12, before peer pressure kicks in and the dreaded addiction cycle begins.
Vaccination? Yes. Understanding It? Not So Much.
While most rangatahi had received their HPV vaccination at school, nearly none knew what it was for. One said: “I just signed the form. I didn’t even know what it was.”
This shows a huge gap in informed consent and health literacy. Our tamariki and rangatahi deserve to know what’s going into their tinana and why.
Primary Care: Cost, Wait Times & Whānau Avoiding Help
Whānau told us loud and clear: “If it’s not for the tamariki, we just don’t go.” The reasons are simple — long wait times and unaffordable costs. Standard GP visits range from $60 to $80, and after-hours care can be as high as $180. Many are turning to emergency departments by default, not because it’s ideal, but because it’s faster and more accessible. For some, the choice between paying rent or seeing a doctor isn’t really a choice — it’s about survival. While telehealth works for a few, unclear pricing has left others feeling misled — one whānau member was shocked when their father’s online consult cost more than an in-person visit.
Cancer Screening: Awareness Growing, But Gaps Remain
Many whānau had been screened for breast, cervical, or bowel cancer, but few had completed all three — and most had to initiate the process themselves, with little guidance from GPs or nurses. A registered nurse told us that while reminders appear in patient files, many health professionals simply overlook them. For wāhine, the screening experience was often described as cold and clinical, lacking cultural safety, with many feeling whakamā — exposed, undignified, and unlikely to return. There was positive feedback too, particularly around cervical screening reminders, which were clear and helpful, and the fast, reassuring turnaround times for breast screening results. However, follow-up care was inconsistent, and whānau made it clear they want more community-based education and engagement — they want to understand what to expect, why it matters, and how to access care before it becomes urgent.
Thank you For Your Truths
We’re deeply grateful to every whānau member and rangatahi who stopped by to share a laugh, a selfie, and a story — your voices are shaping the future of our hauora. Every kōrero is being carried forward in our regular reporting and meetings with Te Whatu Ora. We’re listening, and we thank you for trusting us with your truths.
Hauora at home: Everything under one roof in Whaingāroa
Poihākena Marae in Whaingāroa Raglan was the place to be this week as whānau gathered hauora check-ups, hosted by Toi Oranga in partnership with a range of local and visiting health providers. The open-door event invited whānau to drop in, share a cuppa, and check up on their wellbeing — all in a familiar, friendly environment.
Nurses were onsite offering general health checks, alongside a wide range of services including physiotherapy, mirimiri (traditional Māori bodywork), immunisation, cervical screening, and counselling. A Ministry of Social Development (MSD) staff member was also available.
Two Heart Foundation representatives were kept busy with blood pressure checks, while a local GP provided full consultations in a dedicated clinical space.
Having services close to home made a big difference, particularly for kaumātua who often face challenges accessing care, and for younger whānau looking for convenient, supportive options.
“Whānau felt more comfortable at the marae, and not having to travel far — and having everything under one roof in such a friendly space just made sense,” said Megan Tunks, one of our Whānau Voice kaimahi.
Predominantly Māori came, but some non-Māori as well. “They relaxed with a hot drink and some kai, connected with others, and visited different service providers while they waited.”
Many of the visiting providers, including the physiotherapist and mirimiri practitioners, were from the local community themselves — a powerful reminder of the strength and value of community-led solutions.
The kaupapa was simple and effective: bring health services to where whanau already feel safe, respected, and connected. The result? A whānau-first day grounded in manaakitanga, kaitiakitanga, and whanaungatanga— showing what’s possible when hauora is delivered with aroha.
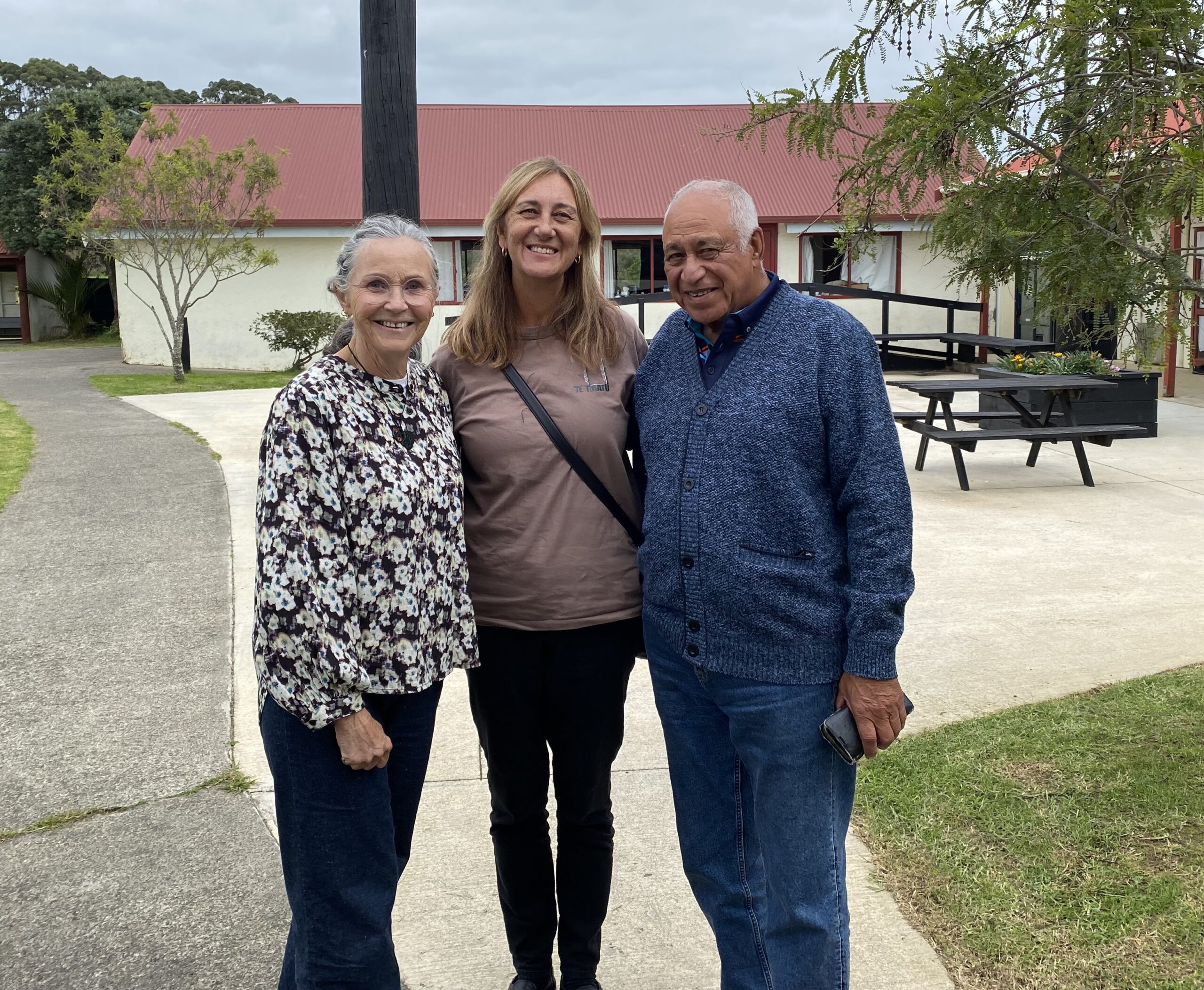
Photo: Lesley Thornley, a physiotherapist and daughter of the late Dr John “Digger” Penman, who served as the local GP from the 1940s to the late 1960s before being succeeded by Dr Ellison; Megan Tunks, Whānau Voice kaimahi with the Te Tiratū Iwi Māori Partnership Board; and Pablo Rickard, affectionately known as Whāingaroa Raglan’s ‘unofficial Mayor’.
From the Frontlines at Waahi Whaanui: Mental Health and Addiction Gaps
On the frontlines of whānau support, the cracks in the system are becoming impossible to ignore.
This week, our Whānau Voice team visited Waahi Whaanui in Raahui Pookeka-Huntly that was established in 1983 by the Tainui Maori Trust Board as one of its ten Marae Cluster Management Committees that works across a vast rohe — from Mercer in the north, to Raglan in the west, Te Hoe in the east, and Kirikiriroa in the south.
They deliver an impressive range of integrated services: Whānau Ora, parenting support, family violence response, social workers in schools, rangatahi transition services, alcohol and addiction support, and more. Deeply embedded in their hapori driven by a commitment to uplift whānau. But even with all their expertise, one reality stood out: they’re doing critical mahi with our people experiencing a health system under immense strain. The need is growing significantly, particularly for our rangatahi.
Mental Health: Access Denied by Distance and Delay
For Raahui Pookeka based whānau,often access mental health assessment is to travel half an hour to Hamilton. Once seen, they’re referred back to local services in Raahui Pookeka—services that are already under immense pressure.
The latest data from Te Hiringa Mahara – Mental Health and Wellbeing Commission backs this up:
- 16,000 fewer people were seen by specialist services in the year to June 2024, compared to 2021.
- More than 10,000 of them were under 25 years old.
- The drop isn’t because fewer people need help—it’s because they can’t get it.
This is a crisis. Not just of access, but of dignity.
Addiction Support Has a Waitlist—But Pain Doesn’t Wait
There’s a four-week wait to see an addiction counsellor at Waahi Whaanui. For some whānau, that’s a tipping point. There is limited alcohol and drug support for rangatahi under 18. We heard that many rangatahi are in crisis, with no place to turn.
Kaumātua Saving Up Their Pain
Kaumātua said they “save up” their health concerns because of cost and not wanting to be hōhā or overburden already stretched services.
It is not tika that they should feel like a burden. They carry our whakapapa, our mātauranga, our mauri. They should be cherished and prioritised.
The Numbers Are Stark—But Not New to Us
Māori in Waikato are:
- 9 times more likely than non-Māori to be hospitalised for any mental or substance use disorder
- 6 times more likely for schizophrenia
- 7 times more likely for substance and alcohol-related harm
- And an average of 225 Māori (mostly wāhine) are hospitalised for intentional self-harm each year
In Hamilton, over 2,000 Māori aren’t enrolled with a GP—shut out from the most basic preventative care.
Where to From Here?
What we saw was a failure of the health system to support providers like Waahi Whaanui who are under pressure, the increased caseload of kaimahi carrying too much without the resources they need, and whānau trying to hold on without falling through the cracks.
We stand alongside them—and we raise their voices.
Last week the Government announced a $28 million investment over four years in Budget 2025 to shift the response to 111 mental distress calls from Police to mental health professionals. For frontline providers like Waahi Whaanui it will take far more to address the deep gaps in accessibility, workforce, and culturally grounded care.
Te Tiratū is calling for:
Providers to be adequately resourced to cope with the increasing demand on services
- A focus on services for rangatahi under 18 that are locally relevant and accessible
- Appropriate whanau orientated triage processes
- Culturally grounded, local solutions led by whānau, hapū and iwi
Te Tiratū will continue to amplify your voice until the system listens.

From left to right: Rawinia Marsh – Integrated Services Manager Waahi Whaanui Trust, Fiona Helu and Hemi-Lee Morgan – Whānau Ora Team.
Maniapoto rising: “We know what works”
Our Whānau Voice kaimahi and Tumu Whakarae attended a recent hui held at Te Kūiti, hosted by Maniapoto Marae Pact Trust where a strong and heartfelt kōrero unfolded about the state of hauora for whānau across the Maniapoto rohe.
Frontline kaimahi, whānau navigators, and community leaders — including CEO Shirley Turner — came together to shine a light on what’s working, what whānau are asking for, and where the system is falling short.
“Our people know what works — we just need the system to back us,” Shirley said.
Maniapoto Marae Pact Trust offers a suite of integrated health and social services designed to walk alongside whānau, ensuring every door is the right door. These include:
- Kaiārahi Services – placing whānau at the centre, helping them define and lead their own goals across multiple service areas.
- Whānau Direct – offering fast, flexible support when whānau need it most.
- Disability support and mental health services, including social workers in schools.
- Tamariki Ora – a standout success story. The Tamariki Ora nurse and whānau navigator work together in the community, achieving strong immunisation rates despite not receiving equitable funding.

Photo from left to right: Te Tiratū Tumu Whakarae, Brandi Hudson with kaimahi of Maniapoto Marae Pact Trust – Sauaga Poliko, Lisa Kerekere, Rena Morgan, Honour Muraahi, Adrianna Astle and Raven Torea our Whānau Voice kaimahi
The Trust also contributes to Healthy Families Te Kūiti, with locals like Michelle Wi running weekly Māra Kai workshops on preserving, pickling, and food sovereignty — all part of a wider push for long-term wellbeing.
Shirley was clear about how the Trust works, “Whānau are in the driver’s seat — and that’s how it should be. Our services walk with them, not ahead of them.”
Systemic Challenges Undermining Equity
Despite these local strengths, systemic failures continue to undermine outcomes for Maniapoto whānau.
One striking example shared at the hui was of a kuia who was rushed by ambulance to Waikato Hospital with minimal belongings, only to be sent home later in a shuttle and left on the roadside.
It was only thanks to a member of the public contacting a local health worker that she made it home safely. This case highlights the urgent need for a more responsive, automatic travel support process — particularly around the National Travel Assistance (NTA) scheme.
“There needs to be a built-in, automatic system for whānau travel vouchers — not an afterthought.”
Other systemic concerns raised include:
- Falling through administrative cracks in post-hospital care and transport.
- No sustainable funding model for high-performing but underfunded services like Tamariki Ora.
- The need for better wellbeing measurement tools that reflect whānau realities.
- A desire for more regular, locally based specialist outreach, especially for kaumātua and kuia.
Networks and Ngā Kaupapa o te Rohe
The hui also acknowledged the strength of local collaborations — such as the Waitomo Community Health Forum and initiatives like Harvest to Home and Wai to Kai, which focus on food resilience, sovereignty, and wellbeing.
The message from Maniapoto is clear: local, kaupapa Māori solutions are working — but they need resourcing and system-level support.
“We’re seeing positive outcomes because our services reflect the lived reality of our whānau. But without equity in funding and process, our people continue to carry the cost,” said one kaimahi.
Rangitāmiro leads the way – First Commissioning Agency to complete Whānau Ora procurement process
PANUI FOR WHĀNAU ORA PROVIDERS
IN TĀMAKI MAKAURAU & TE TAI TOKERAU
21 May 2025, 6:00 PM
2 minutes to Read
Rangitāmiro is proud to announce that it has successfully completed its inaugural Whānau Ora procurement process and today formally notified successful providers across Region One. This is a significant milestone and reaffirms a commitment held by Rangitāmiro to honour the whakapapa of whānau ora through strengthening service networks, regional capability, reach and service coverage, ensuring and enabling whānau wellbeing.
A comprehensive and values-led procurement process that interim Rangitāmiro Chair, Dr Rachel Brown knows will shape the future of Whānau Ora delivery.
“We are honoured to be able to give providers and communities across Aotearoa confidence in the continuation of Whānau Ora services with minimal disruption, whilst ensuring growth in capacity means service reach and coverage will increase allowing more whānau to access the services they need.
Key achievements from this process include:
• Guaranteed continuity of services for whānau from 1 July 2025, with proactive steps to minimise transition disruption
• An increase in frontline Kaiwhiriwhiri Whānau FTE, supporting a stronger navigation workforce across all regions
• Expanded reach into isolated and rural communities, enabling better access to culturally anchored, whānau-centric support
• The onboarding of new providers, bringing fresh innovation, insight, and presence in areas where service gaps previously existed
Dr Brown acknowledges the tenacity of providers and whānau in the short timeframe.
“Today’s announcement signals the next chapter in our partnership with whānau and reinforces our long-term commitment to the transformation and future of Whānau Ora. Our kaupapa is grounded in empowering whānau, driving better outcomes, and expanding service reach to underserved and high-need communities.”
Rangitāmiro is a collaborative entity comprised of Te Tiratū Iwi Māori Partnership Board, the National Hauora Coalition, and Ngaa Pou Hauora oo Taamaki Makaurau Iwi Maaori Partnership Board.

