Ninth wave of COVID-19 arrives
Health services across Aotearoa are reporting a ninth wave of COVID‑19. In the past week, 50 people have been hospitalised and 19 have sadly passed away with the virus.
Most whānau experience mild illness, but our pēpi, kaumātua, and those with existing health conditions remain more vulnerable. Protecting whakapapa is a shared responsibility, and simple actions can make a real difference.
Recent media reports say, “Covid-19 is being tracked through wastewater and hospitalisations which were currently showing a “big wave””.
Simple Steps to Keep Safe
Line up your Covid booster with your annual flu vaccination. Make a booking now.
If you or your tamariki feel unwell with cough, fever, runny nose, or sore throat, stay home, rest, and avoid visiting older whānau or those with health conditions. Testing helps you know if it’s COVID‑19, and free tests or RATs may still be available through local hauora providers or pharmacies.
Vaccination and booster doses build protection and reduce the risk of severe illness, and they are free for most people aged 5 and over. Adults aged 30 and over, particularly whānau Māori are encouraged to stay up to date with boosters when eligible.
Good hygiene continues to help protect everyone. Wash your hands regularly, wear a mask in crowded indoor spaces, and cough or sneeze into your elbow. Staying vigilant helps keep our whānau safe.
Data from Aotearoa shows that our whānau are disproportionately affected by COVID‑19, with higher rates of severe outcomes than other groups. Vaccination and boosters significantly help protect everyone.
Protect Our Whakapapa
Protecting our tamariki and kaumātua by staying home when unwell, testing, isolating if needed, and keeping up with vaccinations saves lives.
Kia noho haumaru e te whānau!

Rangitāmiro reaching more whānau than ever
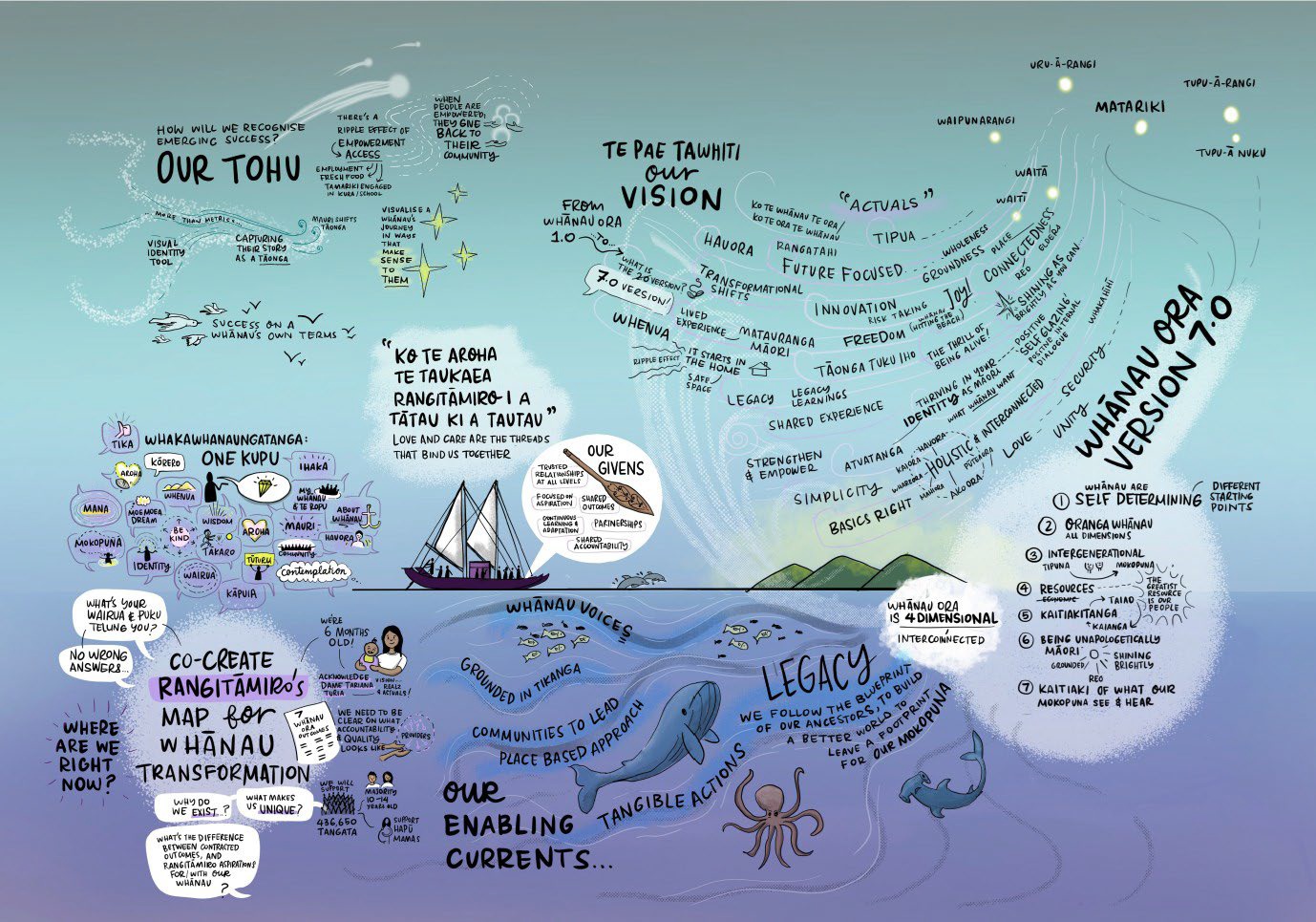
Te Pāe Tawhiti – The shared vision for Rangitāmiro in its journey of evolution from 1.0 toward 7.0
More whānau are connecting with support across Te Tai Tokerau, Tāmaki Makaurau, Waikato and Tūwharetoa as the Whānau Ora commissioning model of Rangitāmiro grows and strengthens.
A quarterly update received today by shareholders for the period October to December 2025 shows growing engagement with whānau and stronger partnerships with providers working in communities across the regions.
The number of whānau engaging with Rangitāmiro services increased over the quarter, rising from 3,228 whānau in October to 3,872 by December.
The whānau-centred approach of Rangitāmiro was especially effective during the recent severe weather events that affected northern regions earlier this year. Working alongside Whānau Ora providers and community organisations, support was coordinated for whānau impacted by the events, demonstrating the strength of kaupapa Māori responses grounded in relationships, tikanga and community leadership.
Support is delivered through Whānau Ora Kaiwhiriwhiri (navigators) who work alongside whānau to help them access services, strengthen connections and achieve their aspirations. Kaiwhiriwhiri across the regions continue to support increasing numbers of whānau seeking guidance and support.
As Rangitāmiro moves beyond its start-up phase, it is continuing to strengthen its systems, workforce and partnerships. Work is underway to grow the capability of Kaiwhiriwhiri across the network, embed the organisation’s mātāpono of whānau, connection and tikanga, and build systems that support continuous learning and improvement.
In November, the Rangitāmiro Board and operational team came together for a strategic wānanga to begin shaping the organisation’s long-term direction. The kōrero focused on a shared vision of intergenerational wellbeing, with tamariki and mokopuna at the centre.
Those attending reflected on what thriving whānau looks like in everyday life, including safe homes, access to kai, learning opportunities, strong cultural identity and connection to whenua and whakapapa. The wānanga also explored the importance of looking ahead seven generations to ensure decisions made today help build a stronger future for mokopuna.
Over the coming months, Rangitāmiro will focus on completing its strategic plan, strengthening data and insights about whānau outcomes, deepening partnerships with providers and continuing to grow support for whānau across the regions it serves.
By grounding its work in tikanga, relationships and whānau voice, Rangitāmiro aims to help whānau realise their aspirations and thrive now and for the next seven generations to come.
Rangitāmiro is a consortium of Te Tiratū Iwi Māori Partnership Board, Ngaa Pou Hauora oo Taamaki Makaurau Iwi Māori Partnership Board and National Hauora Coalition (NHC).
Major health lobby group ‘Kaitiaki Hauora’ backs Iwi Māori Partnership Boards

Kaitiaki Hauora is calling for Te Tiriti o Waitangi to be honoured by empowering Iwi Māori Partnership Boards to lead decisions about health services for their communities.
The national alliance launched in January has brought together patients, health workers, Māori health representatives, unions, advocacy organisations, youth voices, and community groups who share a commitment to protecting and strengthening publicly funded healthcare in Aotearoa.
It is calling for:
- A major boost to funding to meet the real health needs of our population.
- Protecting and strengthening publicly funded and provided healthcare, rather than outsourcing it to private interests.
- Honouring Te Tiriti o Waitangi by devolving decision-making authority and funding to Iwi-Māori Partnership Boards, enabling them to meet the needs and aspirations of their people.
Since launching earlier this year, the Kaitiaki Hauora alliance has grown quickly.
More than 570 people have signed up to support its campaign, and 26 organisations have formally joined the alliance, reflecting strong public support for protecting publicly funded healthcare.
The group has been active in the national conversation about hauora as we experience a critical time for healthcare and the future of the public health system in Aotearoa.
Decisions made by government and Parliament will influence how healthcare is funded, delivered and governed including the role of Māori leadership in shaping services.
For Iwi Māori Partnership Boards, ensuring that Māori voices remain strong in these conversations is essential to achieving equitable health outcomes for whānau.
Kaitiaki Hauora spokespeople include Iwi Māori Partnership Board representation from Chair, Louisa Wall of Tūwharetoa and General Practitioner and Chief Medical Officer of Tūwharetoa Iwi Māori Partnership Board Dr Rawiri Jansen.
Kaitiaki Hauora believes the future of public healthcare will depend on communities working together to protect the system and ensure it reflects the values of fairness, partnership and care for all.
Whānau and organisations in hauora are being encouraged to learn more about the alliance across the motu and how they can support the kaupapa.
Together, the message is clear around kaitiakitanga and kotahitanga. Strong public healthcare and strong Māori leadership must go hand in hand.
Whānau speak up about state of health system at Taumarunui hauora day

Whānau came together this past weekend at Taumarunui Hospital for the annual Hauora Day that was supported by a range of health specialists, community service providers and health teams.
We’d like to tautoko three wahine for their dedication organising this outstanding event. Atarina Peta, a health promoter from Taumarunui, and Willow Brady and Briar Downes from the Screening Team of the Waikato National Public Health Service.
Their leadership created a space where whānau could share their experiences and access vital health support. Community teams included National Hauora Coalition kaimahi, the Te Nehenehenui Health Bus, and the Ngāti Maniapoto Marae PACT Trust who provided information, advice, and resources.
Our Te Tiratū Whānau Voice team listened to whānau in Taumarunui as they shared the realities of accessing healthcare, highlighting common themes of long travel for services, gaps in local care, transport challenges, pressures on mental health and addiction support, and the difficulty many face navigating the health system.
Hāpū Māmā often travel six hours for ultrasounds due to the lack of local facilities, and there is no respite or hospice care available nearby.
Long waits for MRIs, cardiology scans, and GP appointments create stress and anxiety, while pharmacy hours are limited, forcing whānau to travel significant distances for medication. Public transport, such as the health bus, often requires better support, safer conditions, and kaumātua guidance to ensure whānau can travel with confidence.
Mental health and wellbeing were a major focus. Rangatahi anxiety and the pressures on grandparents raising grandchildren due to adult children struggling with meth use were recurring concerns. Many whānau expressed uncertainty about how to support those affected by addiction and highlighted the lack of services for gambling and other behavioural challenges.
The day also revealed gaps in health services, including a need for diabetes programs, sleep clinics, physiotherapy, and rongoā Māori services in Taumarunui. Whānau often face challenges navigating complex health systems, including ICAMS referral processes for infant, child, and adolescent mental health. Reduced Kaitiaki staffing, conflicting medical advice, and inconsistent oral health and counselling services add to the strain.
Despite the challenges raised, whānau also shared positive experiences. Asthma Waikato provided helpful online consultations, Awhi Healthy Homes responded quickly to urgent housing needs, and Te Puawaitanga counselling support was highly valued by those who had accessed it.
Whānau spoke clearly about what they need, like culturally safe services, local advocacy, support to navigate the health system, and more accessible health programmes closer to home.
Taumarunui Hauora Day highlighted both the strength and resilience of the hapori, and the urgent need to improve access to health services locally that Te Tiratū Iwi Māori Partnership Board is exploring further in its soon-to-be-released town-by-town Hauora Report on health access and equity.

Photo: Te Tiratū Iwi Māori Partnership Board kaimahi Megan Tunks of Whānau Voice with Te Whatu Ora kaimahi – Willow Brady , Briar Downs and Atarina Peta who is the Health Promoter based in Taumarunui Hospital.
Koha & water safety kōrero that saves lives with Mark Haimoana

Photo: Megan Tunks of Whānau Voice, Mark Haimoana and Kōare Hudson, Te Tiratū Iwi Māori Partnership Board social media kaimahi.
When Mark Haimoana talks about the moana, he speaks with the mana of someone who has spent a lifetime in it.
Known across Aotearoa for his leadership in water safety, swimming and surfing, Mark has long championed a simple but powerful Kaupapa, that while our people belong in the water, our people must be safe in the water.
For Mark, safety begins long before you reach the shoreline.
The first thing he says is clear. You need to know how to swim. Not just once, not just as a child, but continuously. Swimming, floating, breath control and survival skills need to be practised and maintained.
“Many of us”, he says, “have not dived for a year or more. If you are heading out for a deep dive or even a simple skin dive for kina, pāua or crayfish, you need to be honest about your fitness. The ocean does not lower its expectations because we have been busy or because we are getting older. Preparation is part of respect.”
He also reminds us that in a world where nearly everyone carries a phone, “there is no excuse for silence whānau”. Before heading out on the water, whānau should know where you are going and what time you expect to return.
That simple act of communication can make the difference between a quick response and a long, frightening delay. Letting someone know your plan is not about restriction. It is about care.
Reading the conditions is another expression of that care. The moana is constantly changing. Tides shift, winds turn, swells build. Heading out without checking forecasts or understanding what the water is doing places unnecessary risk on yourself and those who may have to come looking for you.
Mark says, “know your tides, watch the wind and understand how quickly weather can move”. Awareness is protection.
Yet perhaps the most important message he shares is one grounded in our values. “Stay together. Look after each other. Mahi ā whānau.” When we move as a collective, we notice when someone is tired, when conditions feel wrong, when it is time to turn back. Water safety is not an individual pursuit. It is relational.
Mark has kindly donated a lifejacket to Te Tiratū that we will be giving away to whānau on our Facebook page.
It carries that same spirit. It is practical, yes, but it is also symbolic. It represents manaakitanga in action. It says that every life matters, that preventable loss is not something we accept, and that leadership is shown through generosity as much as words.
Te Tiratū Iwi Māori Partnership Board is deeply grateful to Mark Haimoana for this koha and for the decades he has spent strengthening water safety across our communities. As the warmer months draw more of us back to the coast, rivers and lakes, his message is timely.
Skill up. Stay connected. Respect the conditions e te whānau.
Kia haumaru tātou katoa.
Rangitāmiro & shareholders strengthen shared vision

Photo: Governance and operational rangatira of Rangitāmiro with shareholders, Te Tiratū Iwi Māori Partnership Board, Ngaa Pou Hauora oo Taamaki Makaurau Iwi Māori Partnership Board, National Hauora Coalition (NHC)
Board members from Rangitāmiro Whānau Ora Commissioning Agency and its three shareholders, National Hauora Coalition, Ngaa Pou Hauora oo Taamaki Makaurau Iwi Māori Partnership Board, and Te Tiratū Iwi Māori Partnership Board came together in early February to strengthen their shared commitment to improving outcomes for whānau.
The hui brought governance and operational leaders around the same table to reflect on progress, discuss current challenges, and look ahead to the future of investment and support for hapori.
During the hui, Te Tiratū shared insights from its latest quarterly monitoring report on Te Whatu Ora. The report highlighted that many whānau are still facing barriers within the health system. These include long waits to see specialists, delays for surgery, reduced funding for health promotion initiatives, and lower screening rates for some conditions. Gaps also remain in making health information accessible and easy for whānau to understand.
At the same time, there were encouraging signs of progress. Screening rates for cervical and breast cancer have increased by around ten percent, showing the impact of targeted outreach and the strength of community-based engagement. Leaders at the hui reflected on how consistent data, trusted relationships, and clear health messaging all play an important role in helping whānau access care earlier.
Chair of Rangitāmiro, Eru Lyndon, spoke about the importance of maintaining optimism and purpose when working in the social development space.
“Whānau trust the people delivering services and the information they receive, they are more likely to engage with health initiatives such as immunisation, health checks and prevention programmes,” he said. “Building that trust remains one of the most important tasks for those working to support whānau wellbeing.”
The hui also recognised the vital role played by Whānau Ora navigators who walk alongside whānau, supporting them to achieve their aspirations and helping them connect with services, information, and practical support.
Rangitāmiro Chief Executive Te Rōpu Poa provided an update on how Whānau Ora supported communities during the recent cyclone. The kōrero highlighted the critical role marae and hapū play as first responders when emergencies affect their communities.
Leaders emphasised that while immediate support during disasters is essential, building long-term resilience is just as important. Strengthening preparedness and ensuring communities have the support they need to recover and rebuild will remain a key focus moving forward.
Further insight was shared by Te Tiratū board member Dr Mataroria Lyndon, who recently took on the role of Chair of the Independent Investment Board advising Rangitāmiro. He spoke about how the board will help guide equitable and effective commissioning decisions that support whānau wellbeing across generations.
Dr Lyndon also encouraged leaders to think boldly about the future vision for “Whānau Ora 7.0” looking forward seven generations. While the original framework focused on supporting self-managing whānau, he suggested the next phase should aim even higher supporting self-determining whānau exercising tino rangatiratanga, living longer and healthier lives, creating intergenerational prosperity, strengthening economic security through wealth creation, and protecting whenua and the environment through kaitiakitanga.
These whakaaro will help shape future investment priorities and the direction of Rangitāmiro.
Leaders are expected to meet again in May or June to continue building this shared strategy and long-term vision for whānau wellbeing.
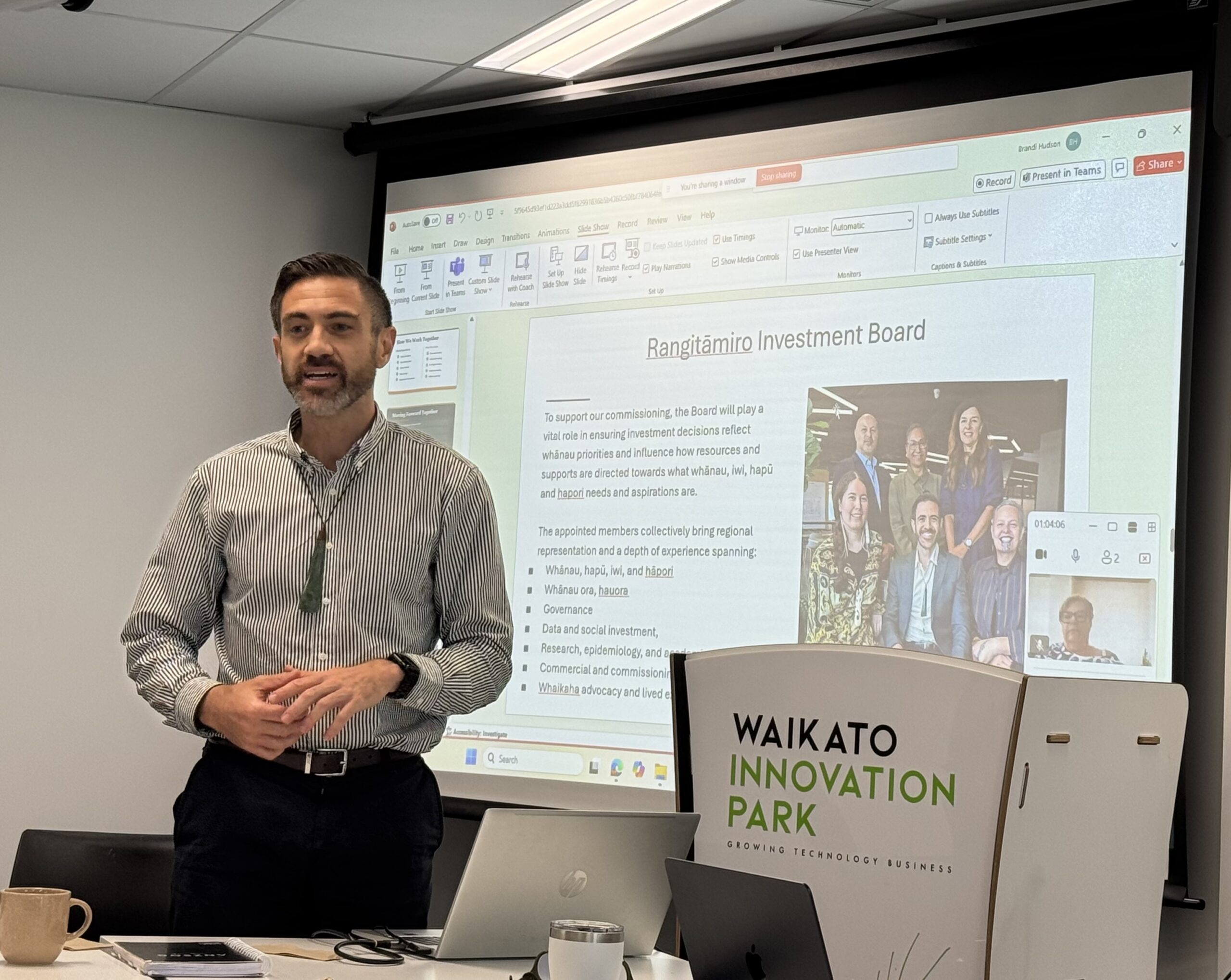
Photo: Te Tiratū Iwi Māori Partnership Board member and Chair of the Independent Investment Advisory Board for Rangitāmiro, Dr Mataroria Lyndon
Changing rangatahi lives in Te Awamutu

Photo: Hauora Team Leader Vinnie Ngaruhe, General Manager Georgina Christie and Raven Torea of Whānau Voice.
Recently, our Whānau Voice kaimahi spent time with Ko Wai Au Trust, a kaupapa Māori rangatahi service grounded in the belief that when young people know who they are, where they belong, and are supported to shape their own futures, they can thrive.
Established in March 2023, Ko Wai Au has grown quickly in response to the needs of rangatahi aged 15 to 24 across Te Awamutu and surrounding communities. Guided by a clear vision to empower rangatahi to live confidently and independently, the Trust places strong emphasis on identity, belonging and practical pathways forward. Its Hauora service, launched under Pinnacle, reflects this by providing accessible, culturally safe health and wellbeing support for rangatahi and their whānau.
Ko Wai Au works closely with rangatahi in schools and in the wider community, often supporting young people who are navigating multiple challenges at once. Their approach centres on early support, strong relationships and walking alongside rangatahi over time. Kaimahi meet rangatahi where they are, building trust and creating space for honest conversations about what is getting in the way of wellbeing, learning or stability.
Support is holistic and rangatahi-centred. Advocacy and mentoring help rangatahi move into education, training and employment, while also supporting them to navigate health, social and justice systems when needed. The team includes youth workers and addiction counsellors who deliver one-to-one support, group programmes and health promotion initiatives that normalise conversations about mental health and reduce stigma.
Much of the mahi focuses on breaking “revolving door” cycles that can keep rangatahi stuck. Practical support with driver licensing, re-engaging in education, first aid certification, life skills and goal-setting helps young people build confidence and independence. Current programmes include Mana Whatu Ahu for rangatahi still engaged in schooling, Tama Ora Tama Tū for those not currently at school, Tu Mahi Toi, walking groups and kai education. Transport is also provided, removing a major access barrier for many rangatahi and whānau.
Strong relationships with local schools underpin the mahi of Ko Wai Au. Trusted partnerships with Cambridge High School, Te Awamutu College and Cambridge College enable early identification of need and coordinated support. Whānau engagement is another strength.
Many parents are working long hours, and a significant number of rangatahi come from low socio-economic households. Ko Wai Au estimates that around 75 percent of the rangatahi they support lack positive role models, making consistent mentoring and trusted adult relationships especially important.
Ko Wai Au also collaborates widely across the local system, including with Rural South mental health services, local GP practices, Cambridge Community Hub, Youth in Tech, and mana whenua partners Ngāti Korokī Kahukura and Maungatautari Marae. These relationships enable rangatahi to access the right support quickly and in ways that feel safe and culturally grounded.
Despite their impact, funding insecurity and housing instability remain significant challenges for rangatahi and for the service itself. From a Whānau Voice perspective, Ko Wai Au demonstrates what works. Kaupapa Māori, relationship-based support that strengthens identity, builds belonging and supports rangatahi to become confident contributors to their communities. Sustainable funding and fair access to commissioning will be critical to ensuring this mahi can continue into the future.
ACC-recognised rongoā in our rohe

Photo: Raven Torea with Whāea Lynette Stafford
Healing grounded in aroha and intention sits at the heart of rongoā Māori. As the whakataukī says, He ringa nā Rongo, he ringa nā te aroha, the hands that heal are guided by peace and care.
The Whānau Voice team recently spent time with rongoā Māori practitioner Lynette Stafford, gaining insight into a healing practice that weaves mātauranga Māori with contemporary therapeutic approaches.
Lynette, known to many as Whāea Lynette, is a rongoā practitioner working through her organisation Te Kora O Mahuika, a Waikato-based provider covering Te Awamutu, Kāwhia, Te Kūiti and Hamilton. Her work takes her across the rohe, and she is in high demand, supporting whānau with injury recovery and wellbeing.
Around 96 percent of Lynette’s mahi is funded through ACC referrals, reflecting growing recognition of rongoā Māori as a legitimate and effective pathway for healing. ACC currently supports rongoā as part of injury recovery, and Lynette is formally trained through Te Wānanga o Aotearoa, where she completed her rongoā qualification. She is also trained in the Emmett Technique, a specialist muscle release therapy that uses gentle finger pressure on specific points of the body to support physical recovery.
Lynette explained that the Emmett Technique is suitable for addressing a wide range of physical and non-physical injuries, and that practitioners must be formally trained to apply it safely. In her practice, this technique often sits alongside rongoā Māori, including rongoā rākau, where native botanicals are used as part of healing. These plants are carefully sourced and applied with knowledge handed down through generations.
For Lynette, rongoā is never “just one thing”. She shared that people sometimes think rongoā is only mirimiri or karakia, but in reality it is a holistic system of healing that includes different forms of treatment, spiritual care, physical techniques, plant knowledge, and deep connection to whenua and whakapapa. In Waikato alone, there are a small number of trained practitioners, each carrying distinct knowledge and approaches.
The visit was especially meaningful for Whānau Voice kaimahai, Raven, who is also a nursing student. Seeing how rongoā Māori and techniques like Emmett can sit alongside Western health practices was new to her and highlights the potential for truly complementary care that centres whānau needs and lived experience.
Time with Lynette reinforced the value of kaupapa Māori healing approaches and the importance of creating pathways where whānau can access care that feels culturally safe, effective, and grounded in who they are. For Te Tiratū and the Whānau Voice team, this visit was a powerful reminder that wellbeing is relational, holistic, and deeply connected to whenua, mātauranga, and whānau.
Pinnacle PHO & Te Tiratū strengthen partnership

Photo: Amit Prasad, Justin Butcher, Glen Tupuhi co-chair Te Tiratū, Brandi Hudson Tumu Whakarae Te Tiratū and kaimahi Rawiri Blundell and Koro Samuels
With a shared commitment to improving Māori health, Te Tiratū Co-Chair and Tumu Whakarae met with Pinnacle Primary Health Organisation leaders Amit Prasad, Justin Butcher, and kaimahi Rawiri Blundell and Koro Samuels to strengthen collaboration on primary care in Waikato.
The kōrero emphasised the importance of all PHOs and Te Whatu Ora working together, particularly by aligning how health data is collected and reported, so decisions are based on accurate, timely information that truly reflects Māori communities at both regional and local levels.
Pinnacle PHO supported our Position Statements and concerns about vaping and its long-term impact on rangatahi and whānau, the critical role of school nurses in proactive healthcare, and the particular challenges faced by rural communities.
There was unanimous agreement that the high number of unenrolled Māori, and those enrolled but not receiving regular health checks or screenings, is an urgent issue that must be addressed collaboratively.
The discussion also highlighted shared pressures in the primary care workforce and the need for sustainable funding solutions. Expanding nurse-led models of care, including mobile services and workplace health checks, was seen as a practical way to reach Māori men and whānau, help address GP shortages, and reduce wait times for appointments.
Strengthening the link between primary care and specialist services was recognised as essential for managing long-term conditions such as cardiovascular disease, diabetes, respiratory illness, mental health, and gout, particularly improving access to prescribed medications. Greater use of Nurse Prescribers was identified as a key way to tackle this pressing equity challenge.
Both organisations acknowledged the importance of supporting whānau to navigate modifiable behaviours, including nutrition, exercise, alcohol use, smoking, and vaping, while ensuring health education resonates with young Māori.
They also recognised that many whānau cannot afford expensive healthy food options, and that solutions must be practical, affordable, and grounded in the lived experience of Māori communities. Lifting immunisation rates remains a shared priority, with a clear focus on closing Māori equity gaps before broader population initiatives.
To maintain momentum and deepen the partnership, a Board-to-Board hui will be scheduled in the New Year. This meeting will advance collaborative work on health data, strengthen advocacy, and guide future investment and planning to achieve better health outcomes for Māori across the Waikato.
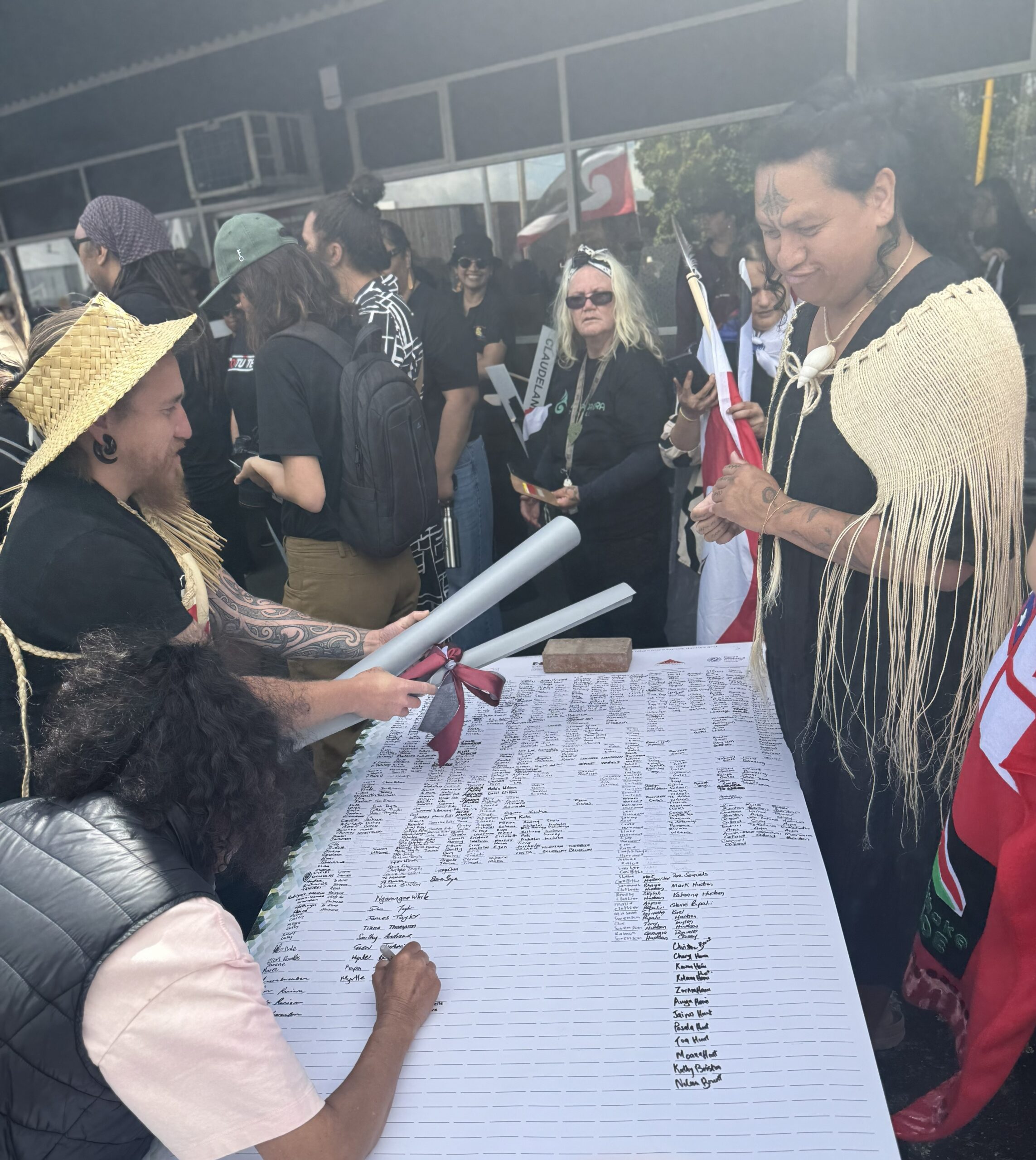
Te Tiratū takes to the streets in Hīkoi for our Health
Several Te Tiratū board members with our senior executive walked in solidarity with hundreds of whānau in the Hamilton leg of the nationwide Hīkoi for Our Health, that’s calling for urgent government action to fix Aotearoa’s failing health system.
The march, led locally by Lady Tureiti Moxon, Managing Director of Te Kōhao Health, departed from Hamilton Lake Playground to Waikato Hospital carrying the Buller Declaration on the State of the New Zealand Health System, now signed by more than 95,000 people.
Our Co-chair Glen Tupuhi, reflected on the responsibility of older generations in protecting the health system.
“It’s very important when we look around and see the rangatahi, and also the baby boomers. It is us that are breaking down. It is us that are putting pressure on the health system, and it is us that really need to fight for the retention of services and not allow this creeping privatisation,” he said.
“Exposing health to free market forces is not going to be good for us, our children, or our tamariki. Our tupuna fought to build the welfare state, and we have inherited that. It’s up to us to ensure it is handed on to the next generation.”
Brandi Hudson, our Tumu Whakarae had a similar stance, “We are here because we want to celebrate the fact that Māori are leading the way with advocacy for better health services for our whānau. We thank Lady Tureiti Moxon today for working alongside the whānau or Kirikiriroa to highlight how the resources for Māori health are failing.”
The focus for Lady Tureiti Moxon is partnership and structural change.
“Te Tiriti o Waitangi is a blueprint for partnership and accountability. When the Crown makes decisions about Māori health without Māori, that is not partnership. We need structural change. This hīkoi is about calling the Government to honour Te Tiriti and build a system designed with, by, and for our people. We walk not just for ourselves, but for our tamariki and mokopuna. For our hauora. For our future,” she said.
Malcolm Mulholland, Chair of Patient Voice Aotearoa and the national organiser, said the hīkoi sends a clear message across the country.
“New Zealanders are united in saying our health system is in crisis. We walk for those behind the statistics, those waiting in corridors, those turned away, and the health workers holding the system together. This hīkoi is our call to those in power: fix it now, before more lives are lost.”
The month-long hīkoi, which began in Westport on 1 November, retraces the path of the original Buller march that sparked this national movement.
It will reach Parliament in Pōneke on Tuesday 18 November, where thousands are expected to gather to deliver the signed Declaration to Members of Parliament. Today in Kirikiriroa, the message was one of unity, mana motuhake, and hope for a health system that values people over bureaucracy and equity over excuses.