Whānau Ora's proof point

Dr Mataroria Lyndon, a board member of Te Tiratū Iwi Māori Partnership Board, has recently been appointed Chair of the Rangitāmiro Whānau Ora Commissioning Agency independent Investment Board, serving 2.3 million people across the upper North Island.
In an interview with Te Ao Māori Editor Mike McRoberts of The National Business Review, he shares his whakaaro on the kaupapa, the responsibility of stewardship, and the strategic mahi ahead to strengthen whānau wellbeing and long-term investment impact.
Explicit safeguards wanted for 12-month prescribing for Māori
For 12-month prescribing to be safe for Māori explicit safeguards are needed, Te Tiratū Iwi Māori Partnership Board says in a Position Statement authored by pharmacist Leanne Te Karu.
Ensuring barriers to access are recognised and removed is key, rather than reduced Māori engagement with their prescriber and medicines by way of a longer prescribing period.
The extended period will work well if it reduces routine GP visits for people with stable conditions, easing pressure on primary care services, but may not provide the same benefits to Māori Tiratū chief executive Brandi Hudson says.
Koha & water safety kōrero that saves lives with Mark Haimoana

Photo: Megan Tunks of Whānau Voice, Mark Haimoana and Kōare Hudson, Te Tiratū Iwi Māori Partnership Board social media kaimahi.
When Mark Haimoana talks about the moana, he speaks with the mana of someone who has spent a lifetime in it.
Known across Aotearoa for his leadership in water safety, swimming and surfing, Mark has long championed a simple but powerful Kaupapa, that while our people belong in the water, our people must be safe in the water.
For Mark, safety begins long before you reach the shoreline.
The first thing he says is clear. You need to know how to swim. Not just once, not just as a child, but continuously. Swimming, floating, breath control and survival skills need to be practised and maintained.
“Many of us”, he says, “have not dived for a year or more. If you are heading out for a deep dive or even a simple skin dive for kina, pāua or crayfish, you need to be honest about your fitness. The ocean does not lower its expectations because we have been busy or because we are getting older. Preparation is part of respect.”
He also reminds us that in a world where nearly everyone carries a phone, “there is no excuse for silence whānau”. Before heading out on the water, whānau should know where you are going and what time you expect to return.
That simple act of communication can make the difference between a quick response and a long, frightening delay. Letting someone know your plan is not about restriction. It is about care.
Reading the conditions is another expression of that care. The moana is constantly changing. Tides shift, winds turn, swells build. Heading out without checking forecasts or understanding what the water is doing places unnecessary risk on yourself and those who may have to come looking for you.
Mark says, “know your tides, watch the wind and understand how quickly weather can move”. Awareness is protection.
Yet perhaps the most important message he shares is one grounded in our values. “Stay together. Look after each other. Mahi ā whānau.” When we move as a collective, we notice when someone is tired, when conditions feel wrong, when it is time to turn back. Water safety is not an individual pursuit. It is relational.
Mark has kindly donated a lifejacket to Te Tiratū that we will be giving away to whānau on our Facebook page.
It carries that same spirit. It is practical, yes, but it is also symbolic. It represents manaakitanga in action. It says that every life matters, that preventable loss is not something we accept, and that leadership is shown through generosity as much as words.
Te Tiratū Iwi Māori Partnership Board is deeply grateful to Mark Haimoana for this koha and for the decades he has spent strengthening water safety across our communities. As the warmer months draw more of us back to the coast, rivers and lakes, his message is timely.
Skill up. Stay connected. Respect the conditions e te whānau.
Kia haumaru tātou katoa.
Lighter paperwork, or better care?
A change to prescription time-frames isn’t a win for all whānau, writes Brandi Hudson.
I understand why some people welcomed the policy change extending the prescribing period to 12 months. It means fewer repeat appointments. Less admin. Less cost. More convenience.
But where I work, at Te Tiratū Iwi Māori Partnership Board, we’re deeply concerned.
Without strong equity and safety safeguards, this change risks widening Māori health inequities, increasing under-care, delaying diagnosis, and causing medication-related harm.
The policy itself sounds tidy. Prescribers can issue prescriptions for up to 12 months for some medicines, while dispensing at the pharmacy still occurs in maximum three-monthly periods. Controlled drugs are excluded. It’s framed as a way to reduce unnecessary appointments and ease pressure on the system.
The trouble is, medicines sit inside real lives. And for many whānau, those lives include multiple conditions, inconsistent access to care, and long gaps between clinical reviews.
It’s easy to imagine a “stable patient” who takes one medicine and has no complications as the basis for policy change. But many of our whānau are managing complex comorbidities, such as diabetes alongside asthma, cardiovascular disease alongside kidney issues, chronic pain alongside depression, and respiratory illness alongside poverty-related stress. Even the presence of two conditions can create risks, interactions, and side effects that need regular review.
For those whānau, prescribing is not just a matter of being told: “Here’s your tablets for the year.” The prescription is part of a care plan that should include monitoring, blood tests, screening, follow-up, and the chance to adjust treatment before harm occurs.
That’s why Te Tiratū supports reducing barriers, but we can’t support a change that reduces the number of touchpoints without putting in place safeguards to protect those who are already missing out.
Māori face significant barriers to accessing medicines. Despite higher rates of chronic conditions such as diabetes, cardiovascular disease and respiratory illness, Māori are overall less likely than non-Māori to access dispensed medicines. In some cases, prescriptions aren’t collected at all because cost, transport, and system barriers make it too difficult.
Extending the length of a prescription doesn’t automatically fix those issues. In some cases, it could even mask them. On paper, a person might look “covered” for 12 months. In reality, they might still be missing doses, skipping follow-ups, not getting blood tests done, or deteriorating quietly until they end up in hospital.
There’s another risk we need to talk about honestly, and that’s the assumption of “clinical stability”.
Who will get labelled stable enough for a 12-month prescription? And who won’t?
In a health system where bias can shape decision-making, sometimes unconsciously, our whānau may be less likely to receive careful follow-up, or more likely to be deemed “fine” without the monitoring that should come with long-term medicines.
Māori don’t experience ill-health in isolation. We live with higher rates of the country’s top five killers — cancer, diabetes, heart disease, stroke and respiratory illness — often all at once. These conditions don’t arrive one by one. They stack, interact, and compound over time.
Add to this the realities many whānau face, such as not always having enough kai, stable housing, or financial security. These are not side issues — they directly affect whether medicines are taken as prescribed, whether follow-up appointments are kept, and whether pain or deterioration is noticed early.
For many of our whānau, poor oral health and chronic foot problems are not minor inconveniences. They affect mobility, sleep, ability to work, and self-esteem. Pain becomes normal. Limited mobility becomes normal. Struggling through becomes normal.
And when complexity becomes normal in a health system under strain, it can quietly slip through the cracks.
Instead of prompting closer monitoring, long-term medicines and complex conditions can be treated as “baseline”. Symptoms are more likely to be interpreted as expected rather than concerning. Whānau may be assessed as “stable” or “fine” not because they’re well, but because their level of unwellness has been unconsciously normalised.
This is how bias can operate without intention. Not through overt neglect, but through lowered expectations of recovery, stability, and follow-up.
Equity in healthcare doesn’t mean treating everyone the same. It means recognising when people are carrying more medical, social, and economic burdens, and responding with more care, not less.
Dr Leanne Te Karu, our expert advisor, has warned that reducing prescribing touchpoints can reduce opportunities to detect deterioration, review side effects, adjust treatment, or optimise medicines. And while community pharmacists are essential, they can’t replace comprehensive clinical review and diagnostic reassessment.
That’s why the solution isn’t simply to provide longer prescriptions. The solution is to build stronger systems around them.
We need national guidance on who isn’t clinically-appropriate to receive a 12-month prescription, and we need equity-focused monitoring that shows what is happening for Māori, not just what is happening on average across the whole population.
We need transparent reporting of adverse events, hospitalisations, medication changes, and wastage. We need Māori-led evaluation of safety, trust, communication and cultural safety.
Most importantly, we need to stop treating medicines as isolated clinical decisions and start treating them as part of a Treaty-aligned system of care.
Te Tiriti obligations of partnership, equity and active protection aren’t optional extras. Partnership means Māori are involved in designing and governing the processes that provide access to medicines, not merely consulted after decisions are made.
Equity means Māori achieve the same access to subsidised medicines and support services as everyone else, with real-world barriers like transport and culturally appropriate information addressed directly. Active protection means outcomes for Māori are monitored, and the policy is adjusted quickly if harm is emerging.
There is a better way forward. Māori pharmacy experts like Dr Te Karu have long advocated for a Te Tiriti-aligned strategy, grounded in Pae Ora and mātauranga Māori, to bring all the right expertise into the room and design medicines pathways that reflect whānau realities, not just administrative convenience.
A 12-month prescription might reduce hassle. But it won’t keep you well if the system stops checking in.
If we want this change to succeed for whānau, we have to measure success by whether Māori are safer, healthier, and better supported — not whether the paperwork got lighter.
Brandi Hudson (Ngāti Maniapoto, Ngāti Rarua, Ngāti Pikiao) is the tumu whakarae (chief executive) of Te Tiratū Iwi Māori Partnership Board, providing strategic leadership across the Waikato rohe to strengthen Māori influence in health system design, planning and service delivery.
She has held senior roles across community, government and not-for-profit sectors, including inaugural CEO of the Independent Māori Statutory Board in Auckland.
Gaps remain in Māori health
The Waikato Local has covered Te Tiratū Iwi Māori Partnership Board’s warning about the 12-month prescription medicine policy change and its potentially adverse impact on whānau Māori as outlined in our Position Statement.
No safeguards for 12-Month prescriptions, Māori health leaders warn
Brandi Hudson, Te Tiratū Tumu Whakarae is warning the Government’s move to 12-month prescriptions could deepen under-care and widen health inequities for whānau Māori unless strong safeguards are built in from day one. Speaking with Waatea she says longer scripts may suit some, but without proper monitoring and follow-up they risk fewer check-ins, delayed diagnosis and worsening long-term conditions. The board is calling for mandatory review points, proactive follow-up systems, culturally safe pathways designed with Māori providers, and real-time data oversight given the policy took effect on 1 February 2026.
Changing rangatahi lives in Te Awamutu

Photo: Hauora Team Leader Vinnie Ngaruhe, General Manager Georgina Christie and Raven Torea of Whānau Voice.
Recently, our Whānau Voice kaimahi spent time with Ko Wai Au Trust, a kaupapa Māori rangatahi service grounded in the belief that when young people know who they are, where they belong, and are supported to shape their own futures, they can thrive.
Established in March 2023, Ko Wai Au has grown quickly in response to the needs of rangatahi aged 15 to 24 across Te Awamutu and surrounding communities. Guided by a clear vision to empower rangatahi to live confidently and independently, the Trust places strong emphasis on identity, belonging and practical pathways forward. Its Hauora service, launched under Pinnacle, reflects this by providing accessible, culturally safe health and wellbeing support for rangatahi and their whānau.
Ko Wai Au works closely with rangatahi in schools and in the wider community, often supporting young people who are navigating multiple challenges at once. Their approach centres on early support, strong relationships and walking alongside rangatahi over time. Kaimahi meet rangatahi where they are, building trust and creating space for honest conversations about what is getting in the way of wellbeing, learning or stability.
Support is holistic and rangatahi-centred. Advocacy and mentoring help rangatahi move into education, training and employment, while also supporting them to navigate health, social and justice systems when needed. The team includes youth workers and addiction counsellors who deliver one-to-one support, group programmes and health promotion initiatives that normalise conversations about mental health and reduce stigma.
Much of the mahi focuses on breaking “revolving door” cycles that can keep rangatahi stuck. Practical support with driver licensing, re-engaging in education, first aid certification, life skills and goal-setting helps young people build confidence and independence. Current programmes include Mana Whatu Ahu for rangatahi still engaged in schooling, Tama Ora Tama Tū for those not currently at school, Tu Mahi Toi, walking groups and kai education. Transport is also provided, removing a major access barrier for many rangatahi and whānau.
Strong relationships with local schools underpin the mahi of Ko Wai Au. Trusted partnerships with Cambridge High School, Te Awamutu College and Cambridge College enable early identification of need and coordinated support. Whānau engagement is another strength.
Many parents are working long hours, and a significant number of rangatahi come from low socio-economic households. Ko Wai Au estimates that around 75 percent of the rangatahi they support lack positive role models, making consistent mentoring and trusted adult relationships especially important.
Ko Wai Au also collaborates widely across the local system, including with Rural South mental health services, local GP practices, Cambridge Community Hub, Youth in Tech, and mana whenua partners Ngāti Korokī Kahukura and Maungatautari Marae. These relationships enable rangatahi to access the right support quickly and in ways that feel safe and culturally grounded.
Despite their impact, funding insecurity and housing instability remain significant challenges for rangatahi and for the service itself. From a Whānau Voice perspective, Ko Wai Au demonstrates what works. Kaupapa Māori, relationship-based support that strengthens identity, builds belonging and supports rangatahi to become confident contributors to their communities. Sustainable funding and fair access to commissioning will be critical to ensuring this mahi can continue into the future.
ACC-recognised rongoā in our rohe

Photo: Raven Torea with Whāea Lynette Stafford
Healing grounded in aroha and intention sits at the heart of rongoā Māori. As the whakataukī says, He ringa nā Rongo, he ringa nā te aroha, the hands that heal are guided by peace and care.
The Whānau Voice team recently spent time with rongoā Māori practitioner Lynette Stafford, gaining insight into a healing practice that weaves mātauranga Māori with contemporary therapeutic approaches.
Lynette, known to many as Whāea Lynette, is a rongoā practitioner working through her organisation Te Kora O Mahuika, a Waikato-based provider covering Te Awamutu, Kāwhia, Te Kūiti and Hamilton. Her work takes her across the rohe, and she is in high demand, supporting whānau with injury recovery and wellbeing.
Around 96 percent of Lynette’s mahi is funded through ACC referrals, reflecting growing recognition of rongoā Māori as a legitimate and effective pathway for healing. ACC currently supports rongoā as part of injury recovery, and Lynette is formally trained through Te Wānanga o Aotearoa, where she completed her rongoā qualification. She is also trained in the Emmett Technique, a specialist muscle release therapy that uses gentle finger pressure on specific points of the body to support physical recovery.
Lynette explained that the Emmett Technique is suitable for addressing a wide range of physical and non-physical injuries, and that practitioners must be formally trained to apply it safely. In her practice, this technique often sits alongside rongoā Māori, including rongoā rākau, where native botanicals are used as part of healing. These plants are carefully sourced and applied with knowledge handed down through generations.
For Lynette, rongoā is never “just one thing”. She shared that people sometimes think rongoā is only mirimiri or karakia, but in reality it is a holistic system of healing that includes different forms of treatment, spiritual care, physical techniques, plant knowledge, and deep connection to whenua and whakapapa. In Waikato alone, there are a small number of trained practitioners, each carrying distinct knowledge and approaches.
The visit was especially meaningful for Whānau Voice kaimahai, Raven, who is also a nursing student. Seeing how rongoā Māori and techniques like Emmett can sit alongside Western health practices was new to her and highlights the potential for truly complementary care that centres whānau needs and lived experience.
Time with Lynette reinforced the value of kaupapa Māori healing approaches and the importance of creating pathways where whānau can access care that feels culturally safe, effective, and grounded in who they are. For Te Tiratū and the Whānau Voice team, this visit was a powerful reminder that wellbeing is relational, holistic, and deeply connected to whenua, mātauranga, and whānau.
Te Tiratū Iwi Māori Partnership Board member named new chair
Our Board member and clinician, Dr Mataroria Lyndon (MBChB, MPH, PhD), is the newly appointed Chair of the Whānau Ora Investment Board for the Upper North Island. He speaks to Waatea about the Board’s vital role in directing government resources to support whānau wellbeing. Under her leadership, the Board will continue to champion locally driven, culturally aligned initiatives that deliver sustainable, long-term outcomes for whānau across Aotearoa.
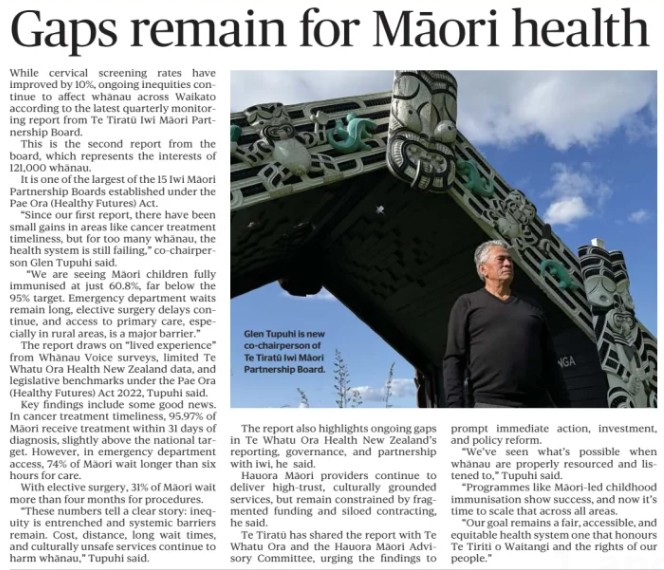
Gaps remain in Māori health
The Waikato Local has covered Te Tiratū Iwi Māori Partnership Board’s latest Quarterly Monitoring Report on the health system, which highlights persistent health inequities for Māori across the Tainui waka rohe. While small gains were seen in cervical screening and timely cancer treatment, major gaps remain: only 60.8% of Māori children are fully immunised at 24 months, long emergency department waits affect 74% of Māori, and nearly a third face elective surgery delays over four months. Co-Chair Glen Tupuhi calls for immediate action, investment, and scaling of Māori-led health initiatives.