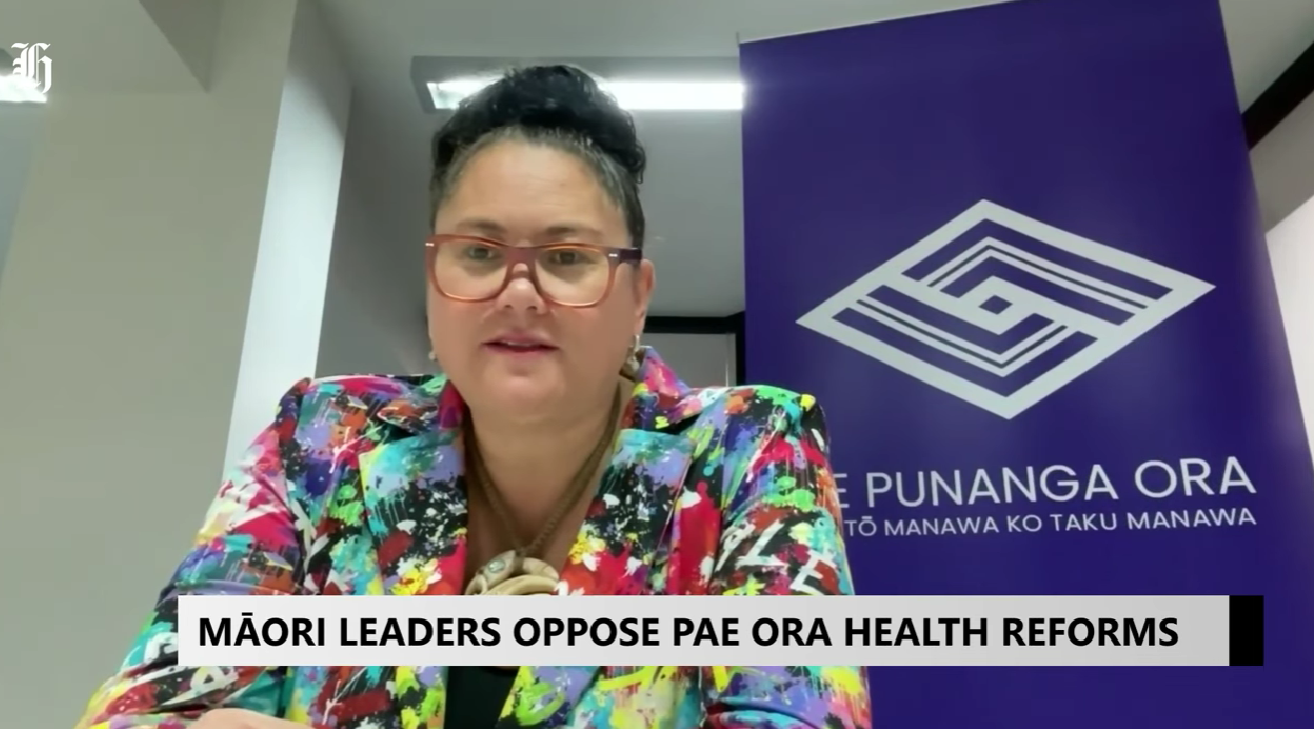
Māori leaders oppose Pae Ora health reforms
Photo: Te Manawa Taki IMPB collective member, Tūwharetoa Iwi Māori Partnership Board Chair Louisa Wall at the National IMPB hui
All 15 Iwi Māori Partnership Boards (IMPBs) gathered in Taranaki to oppose proposed amendments to the Pae Ora (Healthy Futures) Act, warning the changes would significantly reduce their role, including removing critical monitoring powers. Louisa Wall, Chair of Tūwharetoa Toa IMPB, when interviewed by HeraldNOW, explained that IMPBs were created following the Waitangi Tribunal’s 2019 recommendation and the Simpson Review to address systemic inequities, including institutional racism, and to ensure Māori voices shape health services.
Wall said that Māori often access healthcare too late, and IMPBs are uniquely positioned to support preventative initiatives, immunizations, and screenings through a Māori, rural, disability, and patient-centered lens. She criticized the government’s move to shift authority to the Minister-appointed Hauora Māori Advisory Committee, saying it cuts iwi and hapū out of decision-making and undermines the partnerships that are essential for transforming the health system and improving equity for all New Zealanders.
What whaanau told us at Tainui Hui-aa-Tau

Photo: Whaaea Audrey Wildermott, Ngaati Koroki Kahukura with Whaanau Voice kaimahi
Te Tiratū Iwi Māori Partnership Board was honoured to attend Tainui Hui-aa-Tau 2025, hosted by Tainui iwi walking in the steps of their visionary Koiora strategy. This aspirational kaupapa brought together thousands of uri and providers across the motu to connect, share, and strengthen collective oranga.
We were there by invitation to support Whaanau Voice and deepen our understanding of how the Koiora Collective and Te Tiratū fit within the wider ecosystem of Māori health and wellbeing. While our original focus was on promoting our Oranga Survey the day quickly turned into something more — a space for heartfelt koorero and deep listening.
What we heard was despite government targets focused on faster cancer treatment, shorter ED stays, improved immunisation, and reduced wait times for specialist and elective care, whaanau at Tainui Hu-a-Tau described a system that remains slow, hard to access, is culturally disconnected, and difficult to navigate — especially for whaanau seeking kaupapa Maaori services and timely, affordable care.
Whaanau Voice Leads the Way
Our space at Hui-aa-Tau was a hive of activity, filled with whānau keen to share their experiences and insights about accessing healthcare. Many whaanau wanted to koorero at length, reflecting a widespread desire to be heard. Primary care was a consistent topic. Whānau spoke about long GP wait times, often up to four weeks, difficulty enrolling at kaupapa Maaori clinics due to capped rolls, and the frustration of not being able to see the same doctor for continuity of care. Many whaanau living rurally shared feelings of isolation from healthcare, relying on transport support from whaanau, iwi or local services. For those who could afford it, urgent care was preferred over long waits at emergency departments, but even this came with financial strain.
The Strain of Financial Pressure
Cost was a major barrier. Whaanau shared stories of having to choose between kai and seeing a doctor. Prescriptions added another burden. Even if a whaanau member managed to secure an appointment, the costs didn’t end there. Some spoke of giving up altogether — delaying care or avoiding it until it became urgent. Many whaanau weren’t enrolled with a GP at all. Some had been trying to enrol with kaupapa Maaori services but were turned away due to capacity limits. Several questioned why non-Maaori were enrolled in Maaori-specific services when they, as tangata whenua, were being declined. There was deep mamae in these koorero, and a desire for a fairer, more culturally grounded system.
The Challenge of Health Literacy for Kaumatua
Kaumatua shared personal journeys of navigating health conditions and the system without proper explanations or support. One kaumatua described an 18-month journey to get assistance to help manage his diabetes to get it under control which is a long time to be mauiui. Others expressed confusion around medication or what services were available to them. Many didn’t know where to go or how to ask for help, and several mentioned feeling whakamaa about not understanding their conditions. The language barrier was another big one, where whaanau are not able to understand a lot of different accents by non-Maaori health practitioners, they feel there is a lack of cultural safety too. For kaumatua living rurally, transport remains another major barrier. Many said that it was much easier for them to go to their local marae that was close. Many rely on once-a-week iwi transport or local hauora hubs that have now been scaled back due to funding cuts. In some areas, services that once operated five days a week now open for just one — creating high demand and limiting access.
Mental Health in Crisis
Mental health was another area of concern. Many who spoke were supporting a sibling, cousin or other whaanau member. The main issue raised was the lack of support available before a person reaches crisis or hospitalisation. Henry Bennett Centre came up repeatedly — described as difficult to deal with, lacking cultural safety, and disconnected from whaanau. Whaanau described not being informed about loved ones’ care, feeling shut out of the process, and being left to advocate for their whaanau without support.
There was a strong call for mental health services that are proactive, culturally safe, and easy to navigate. Many felt stuck trying to get help for their whaanau and repeatedly faced barriers in the process.
The Hidden Gaps in Women’s Health
A number of wahine raised concerns about the lack of accessible information around menopause. They described debilitating symptoms and feeling unsupported or dismissed. Some were surprised to learn just how little was publicly available in terms of education and care. The koorero made it clear that more kaupapa Maaori women’s health services are needed — both in delivery and in design.
Hearing Loss, Delayed Care and Advocacy
Hearing support was another unexpected but prominent theme. Many whaanau attending the hui wore hearing aids, yet no hearing-focused service was present. One kaumatua, a veteran of the New Zealand Army, shared that it took years to realise the extent of his hearing loss. Another wahine described the two-year process of trying to get care for her daughter — eventually only made possible with the help of a Maaori advocate. For these whaanau, accessing support required determination, energy, and navigating complex systems. Funding options, eligibility, and appointment access created further layers of stress. Even for tamariki, care was delayed — sometimes for years. While support grants like the kaumatua hearing aid fund exist, awareness and accessibility remain major gaps.
The Need for Rongoaa and Kaupapa Maaori Options
Throughout the day, whaanau called for more access to mirimiri and rongoaa Maaori. There was a hunger for services that reflect maatauranga Māori and are grounded in whakapapa and whaanau values. One whaanau member, supporting a younger relative who had experienced a stroke, spoke of the lack of Maaori-led recovery options. Others expressed interest in alternatives to mainstream medication but didn’t know where to start. The desire for Maaori-led, whaanau-centric, culturally affirming care was one of the strongest themes to emerge. It aligns closely with the aspirations of Tainui’s Koiora strategy and the values Te Tiratū holds as we walk alongside whaanau and providers.
A Call to Honour Whaanau Voice in System Change
Tainui Hu-aa-Tau 2025 was more than an event — it was a collective pulse check on how the health system is serving our people. Whaanau were open, honest, and generous with their koorero. Their insights paint a clear picture of a system that needs to evolve, one that genuinely centres Whaanau Voice, upholds Te Tiriti o Waitangi, and recognises hauora as a right, not a privilege. We are committed to carrying these voices forward — into our planning, our advocacy, and our partnership with Te Whatu Ora. We also mihi to Tainui iwi for their bold leadership and vision, and for the opportunity to stand together in kaupapa Maaori-led transformation. Te Tiratū will continue to listen and act — because when whaanau speak, the system must listen and respond.
"Kāore e taea te whakamāhara i tēnei wā” – Kura rata hou ki Waikato
Kua whakaaetia e te kāwanatanga he pūtea mō tētahi kura rata hōu ki Te Whare Wānanga o Waikato, ka whakatūria hai te tau 2028.
Ka whakangungua e tēnei kura ngā rata hōu mō ngā hapori tuawhenua me ngā rohe kāore i te pātata ki ngā ratonga hauora.
Hai tā te Tiamana takirua i te Poari o Te Tiratu, e ai ki a Hagen Tautari, ko te mahi mā Te Tiratu ki te kura rata ko te whakatō i ngā wāriu Māori hai pae ārahi i ngā whakahaerenga katoa, mā reira e ū ai te kura ki ngā mātāpono o te ao Māori.
Healthy Futures (Pae Ora) amendment Bill passes first reading
The Healthy Futures (Pae Ora) Amendment Bill aimed at reforming the Pae Ora (Healthy Futures) Act 2022 has passed its first reading in Parliament. The legislation was introduced by Health Minister, Hon. Simeon Brown who says it “puts patients first”. He described the reforms as a move toward “less Wellington waffle, more results,” with legislated specific health targets, stating “what gets measured gets managed.”
Opposition MPs from various parties strongly criticised the Bill during its first reading, warning it would roll back Māori health equity, strip Te Tiriti o Waitangi commitments, and shift the system away from prevention and public wellbeing. All-in-all it was “devastating” to the aspirations of Māori.
While acknowledging the need to improve hospital wait times and workforce pressures, MPs argued that reform should not come at the cost of Māori-led solutions or equity. They condemned the removal of Te Tiriti obligations, how Iwi Māori Partnership Boards have become advisory roles, and the loss of Māori health targets — describing it as an attempt to “whitewash” Māori governance.
Broad opposition across the sector was also raised in the House which spanned Māori and non-Māori organisations — including the National Iwi Chairs Forum, PSA Māori Caucus, Hauora Māori groups, and Waitangi Tribunal claimants.
Several experts, including Dame Naida Glavish, Professor Sue Crengle, and Dr Rawiri Keenan, labelled the Bill a “direct attack on Māori wellbeing”, with Keenan calling it “ethnocide.” Opposition speakers also highlighted the key role iwi and Māori providers played during COVID-19 for all of society and warned that their leadership was now being undermined.
Members also said the Bill shifts the system’s focus from Pae Ora (healthy futures) to Pae Mate (illness), weakening prevention and population health strategies. They also accused the Government of politicising the public sector and offering hollow praise for health workers amid ongoing workforce burnout and departures to Australia. Opposition leaders vowed to repeal the Bill if elected in 2026.
The Bill will now go to select committee for public submissions. It will report back on 25 November 2025.
'We cannot miss this moment': Waikato medical school must address health inequities - iwi
Te Tiratū Iwi Māori Partnership Board welcomes the Government’s $82.85 million investment in the new medical school at the University of Waikato, due to open in 2028 with an initial intake of 120 students.
Representing 114,000 whānau Māori in the region, Te Tiratū says this is a once-in-a-generation opportunity to tackle long-standing health inequities and workforce shortages—especially for rural, Māori and underserved communities.
Co-chair Tipa Mahuta emphasises that the school must embed Māori health workforce development, cultural safety, and equity from the ground up. “Cultural safety is not optional—it is essential for trust, clinical excellence, and better health outcomes.”
Co-chair Hagen Tautari adds, “A third medical school must reflect a culturally grounded, equity-driven model that serves those most in need.”
Te Tiratū stands ready to partner with Te Whatu Ora, Hauora Māori Directorate, the University of Waikato, iwi and hapū to shape a future-focused medical school that delivers for Māori.
Third medical school must deliver for Māori – Te Tiratū welcomes $83M Waikato investment
MEDIA STATEMENT
FOR IMMEDIATE RELEASE
Friday 22 July 2025, 8:00 AM
2 minutes to Read

Image credit: Waikato Te Whare Wānanga o Waikato. An artist’s impression of the new Division of Health Precinct, which will be home to the New Zealand Graduate School of Medicine at the Hamilton campus.
Te Tiratū Iwi Māori Partnership Board representing 114,000 whānau Māori in Tainui waka rohe welcomes the Government’s announcement of $83 million in public funding, alongside philanthropic and university support, for the new Graduate School of Medicine at the University of Waikato Te Whare Wānanga o Waikato.
This investment marks a significant opportunity to address long-standing health inequities and workforce shortages in our region—especially for rural, Māori and underserved communities.
But this can only be realised if Māori health workforce development, cultural safety, and equity are embedded as foundational pillars in the new medical school’s design, training model, and governance.
“Whānau across Waikato have told us time and again: they want to see more Māori health professionals—people who understand our values, our lived experiences, and our ways of being as Māori,” said Tipa Mahuta co-chair of Te Tiratū Iwi Māori Partnership Board.
Māori currently make up less than 5% of the medical workforce, despite representing around 17–18% of the total population — a stark gap that highlights the urgent need for a more representative and equitable health system.
“Cultural safety is not a nice-to-have. It is essential to clinical excellence, trust, and good health outcomes. If patients don’t feel safe, they disengage—and that can cost lives,” Mahuta added.
The Te Tiratū Community Health Plan, Priorities Report, Monitoring Report, and Whānau Voice insights highlight critical barriers to care in the region:
- A lack of Māori-led service delivery options
- Inadequate rural and specialist services
- Persistent racism, judgement and cultural disconnection in some mainstream settings
Whānau are calling for a health system that is fair, accessible and reflective of the communities it serves. This means:
- A representative medical workforce that includes more Māori doctors, nurses, prescribers, dental/oral health professions, midwifes, therapists, mental health clinicians, sonographers, pharmacists, radiologists, anaesthetic technicians and specialists
- Clinical training of doctors grounded in kaupapa Māori values and culturally safe practice
- Data transparency and partnership with iwi and IMPBs in shaping workforce investment decisions
- Recognition of all hauora roles—from kaiawhina to clinicians—as part of a thriving Māori health ecosystem
As of 30 June 2025, there are 3,991 Māori registered with the Kia Ora Hauora the Māori health workforce development programme nationally. 240 identify with at least one iwi from Waikato. Yet many are still met with barriers, not bridges, into medical and health professions.
Te Tiratū urges the Government, Te Whatu Ora Health New Zealand, Hauora Māori Directorate and the University of Waikato to work closely with iwi, hapū and community partners to shape a graduate school that delivers on its promise—not only to grow the GP workforce of clinical placements across the country, but to heal a system given Māori die on average at least 7 years before non-Māori.
“We cannot miss this moment. A third medical school must reflect a third way—a culturally grounded, equity-driven, future-facing model of training that serves all New Zealanders, starting with those most underserved,” co-chair of Te Tiratū Iwi Māori Partnership Board, Hagen Tautari said.
Te Tiratū stands ready to partner and contribute to the new ‘Division of Health’ health precinct opening on the University of Waikato Te Whare Wānanga o Waikato campus.
The Board, under its statutory role in accordance with the Pae Ora Act, actively reflects and advocates for local Māori views on how public health services and public health initiatives are shaped and implemented.
The Board represents the whānau of Pare Hauraki, Waikato, Raukawa, Te Nehenehenui, Ngāti Hāua (Taumarunui) and Te Rūnanga o Kirikiriroa from the localities of Waikato, Hauraki, Maniapoto, Raukawa, Ngāti Hāua.

Kia Ora Hauora sees Waikato Tainui as a key strategic Iwi relationship within the Waikato region.

Programme Statistics – see overall Kia Ora Hauora statistics and statistics for Te Tiratū specifically.
Rangatahi straight-up truths about hauora

Photo: Rangatahi Mokoia Hamiora-Houghton, the Kaitautoko/Kaitiaki of students from Rototuna High School attending the Kapa Haka and a Taiohi forum organised at Claudelands by Te Puna Wananga o Wairere.
Our rangatahi aren’t just open to kōrero—they’re confident, articulate and have important whakaaro that health leaders must listen too. In June, 96 chose to share their views through Whānau Voice surveys gathered both online and face-to-face. Combined with broader findings from our Community Health Plan, first Monitoring Report, and engagement activities between March and June, their voices offer powerful and direct insights into the health and wellbeing issues they care about most.
While many rangatahi were unfamiliar with some medical terms—particularly questions around the HPV vaccine—they showed curiosity and deep interest in learning more once questions were explained in plain language. What followed was a series of straight-up reflections that reveal the aspirations and challenges our young people face every day.
Mental health emerged as the number one concern. A third of all respondents saying they want more support and information in this space. Sexual health was another key area, especially among rangatahi worried about teen pregnancy and gaps in knowledge. Nutrition, the rising cost of healthy food, the dangers of vaping, and curiosity about rongoā Māori also featured strongly.
Here’s some of what they said:
- “Mental health & the dangers of vaping.”
- “As there’s so much teens who are hapū I feel like there needs to be more health info regarding sexual health and pregnancy.”
- “Nutrition info, particularly considering veggies and fruit are so expensive.”
- “More info about mirimiri in general would be awesome.”
What would help rangatahi stop – or not start – vaping? A lot of rangatahi told us they had tried vaping or were still vaping, even those as young as 12–17. They’re worried about how easy it is to access vapes, and many felt there should be tighter rules – like bans, stricter age checks, less advertising and more support.
Some of their whakaaro:
- “Ban vaping”
- “More restrictions, not advertising, and explaining the danger”
- “Need ID to purchase. There are places you don’t need it”
- “Give out methanol mints to encourage them to stop vaping”
Almost one in four said vaping should be banned or more tightly restricted. They also pointed to peer pressure as a key driver, and many said more mental health support and access to alternative activities—like sport, music, or creative outlets—would make a real difference.
“It’s the popularity of it, if mates do it others will too,” one rangatahi said.
Do rangatahi know about the HPV vaccine? Just over half had heard of the HPV (Human Papilloma Virus) vaccine. But nearly a third hadn’t, and some weren’t sure. It highlighted a mixed picture around the HPV vaccine. A significant number weren’t sure if they’d even been offered the vaccine at all, showing that school-based communication and consent processes may need strengthening. Even among those who had the vaccine, many still lacked clear understanding about what the vaccine is, why it’s important, or what it does in their bodies. This shows there’s still a big gap in the way health info is shared with our rangatahi – and it’s something we can work together to improve.
This kōrero with rangatahi reminds us that they are thoughtful, brave and full of ideas. When we take time to kōrero properly, they show up and are ready to lead, if we’re willing to listen. Their insights call for us—whānau, schools, health providers, and communities—to create safe space for deeper conversations and to ensure our health systems are reaching them with the right tools, messages, and manaakitanga. Our rangatahi have the answers. It’s time we act on them.
What’s really happening with cancer screening our rohe

Cancer impacts countless whānau across Waikato—and feedback from 23 whānau within the Tainui waka region, together with broader insights from our Community Health Plan, initial Monitoring Report, and engagement efforts from March to June, is revealing what’s effective, what’s falling short, and where services need to improve.
Our first Monitoring Report, released this month, shows that breast screening rates for wāhine Māori in Waikato continue to lag behind. Currently, just 54.5% of our wāhine are up to date with screening—7% lower than the national rate for non-Māori (64.6%). While there has been a small improvement of 1.1% since the last quarter, the pace of change remains too slow to close the equity gap.[1]
Most surveyed by our Whānau Voice team (nearly 74%) told us they regularly take part in cancer screening, particularly breast and cervical checks. Many said this is driven by personal or whānau experience of cancer. One participant shared: “My mum had cancer… I made self-referrals. I know how important it is to catch it early.”
But behind those statistics lies a more complex picture. Screening isn’t always comfortable. Over half of respondents said the process left them feeling whakamā, exposed, or in pain. Several described experiences that were rushed or poorly explained—leaving them uncertain, anxious, or unlikely to return. One woman shared: “Didn’t want to go back after last time—felt exposed.” Another added: “It was painful and no one explained anything.”
This discomfort was often made worse by a lack of cultural safety. Māori participants talked about mispronounced names, feeling spoken over, or being asked sensitive questions without privacy. “The lady at reception was white and made no effort to pronounce my Māori name,” said one. Others spoke of rushed appointments and the feeling that their experience wasn’t respected or mana-enhancing.
Not everyone receives timely results, either. Some whānau said they had to chase clinics for updates, while others described waiting months for treatment—even when a diagnosis had already been made. One respondent noted: “We waited 3–4 months, even with private insurance. Treatment took 6–9 months. Too long.”
The good news? Whānau know what would help.
They asked for more Māori doctors and support workers, better access to information, and culturally grounded care that includes warm, respectful service and more whānau-friendly settings—like marae, mobile clinics, or iwi spaces. Many called for free screening for kaumātua, flexible appointment times, and reminders by text or email, noting that these are not offered consistently.
Suggestions were practical and clear:
- “More Māori health professionals, please.”
- “Better-informed and pre-screening promotion.”
- “Use marae and iwi groups to get the message out.”
- “Have a Māori support person due to the medical language.”
A little over half of those surveyed also had a whānau member diagnosed with cancer in the last three years, and nearly half of them said they did not receive enough information about the treatment journey or support services.
There’s a clear call here—not just for more education and outreach, but for services that genuinely listen, respond, and hold space for whānau with care. As one whānau put it: “We need more manaaki-focused care. It makes all the difference.”
This kōrero reinforces the need for screening services that don’t just invite people in but hold them with dignity, understanding, and culturally safe support. Because early detection saves lives—but only if our people feel safe enough to walk through the door.
[1] Pg 13 Source: https://tetiratu.co.nz/wp-content/uploads/2025/07/2025-Te-Tiratu-IMPB-Monitoring-Report-to-March-2025.pdf
GP door closed for many: Whānau speak out

Photo: Kuia providing feedback at a recent Taumarunui Hapori Hauora Day
“We waited eight hours, and no one even told us how long it would be.”
This is the reality for many Māori whānau in the Waikato region, as shown in the latest Whānau Voice quarterly results that reveals the deep cracks in our primary care system.
These insights are drawn from a snapshot survey completed by 88 participants, alongside wider data gathered through our Community Health Plan, first Monitoring Report and engagement activities held between March and June. Their voices paint a clear picture judging by the indicative results, that our local health system is under immense pressure, and it’s pushing whānau to breaking point.
Despite more than 90% of respondents being enrolled with a regular GP, nearly 40% said they were unable to get an urgent appointment when they needed one. For many, the GP door feels effectively closed—whether due to fully booked clinics, high costs, or services being unavailable altogether.
In the first Health System Monitoring Report by Te Tiratū released this month, we note that key data from Te Whatu Ora is still missing. This includes:
- GP enrolment figures compared to the population (Māori vs non-Māori by age)
- Māori utilisation of GP services over the past 12, 24, and 36 months
- Māori utilisation by type of service (in-clinic vs virtual)
This lack of data limits our ability to assess equity in access and use of primary care services for Māori.[1]
So, in these moments of urgency, whānau are being forced to turn to urgent care clinics or hospital emergency departments for care that should be delivered by a GP. Nearly three-quarters of those surveyed said they had gone to A&E when they couldn’t get a GP appointment.
Of those, 29 percent reported waiting six to eight hours. Nine percent said they waited more than ten hours. Most waited without receiving any updates or basic information—86 percent received no health information during their wait, and 84 percent weren’t told how long the wait would be.
Adding to the strain, more than half of respondents said cost had stopped them or their whānau from getting care. This was particularly true for those in remote or rural areas like Tokoroa, Waharoa, and Huntly, where choices are limited and even getting to a clinic can be a challenge.
Some whānau reported being unable to enrol with a GP because no clinics were accepting new patients, or they lacked the required ID. These are not isolated stories; they reflect systemic barriers that need urgent attention.
What is Working?
Not all findings were bleak. Most people reported being able to get planned appointments when needed, and those who used telehealth services found them useful—90 percent said the advice met their needs.
Enrolment in a regular general practice remains high, which shows that there is a foundation to build from. But trust and consistency remain issues, with more than half saying they don’t get to see the same doctor each time.
This survey doesn’t just reveal long wait times or stretched services—it highlights the emotional weight of a system that too often leaves Māori whānau out of reach. It tells a story of people navigating closed doors, cost barriers, and uncertainty, just to access the care they deserve.
Te Tiratū Iwi Māori Partnership Board is using this data to advocate for urgent investment in services that are responsive, affordable, and culturally safe. Because no one should have to wait ten hours in an emergency room for care that should have been delivered in a clinic—least of all our tamariki and kaumātua.
[1] Pg 4 Source: https://tetiratu.co.nz/wp-content/uploads/2025/07/2025-Te-Tiratu-IMPB-Monitoring-Report-to-March-2025.pdf
It’s a confronting wake-up call
Photo: Te Tiratū Iwi Māori Partnership Board Co-chair Hagen Tautari
TVNZ’s Te Karere has aired a powerful segment on a new report from the Te Tiratū Iwi Māori Partnership Board, describing it as a “confronting wake-up call” for Aotearoa’s health system. The Board’s first-ever health system monitoring report reveals that Māori are still dying seven years earlier than non-Māori, with many of those deaths preventable.
The story highlights long waits, high costs, unsafe care, and poor screening rates as signs of a system that continues to fail Māori. “All of us, in particular with government, they need to ensure that the funding is adequate to protect our people,” said a Board representative. “We (Iwi Māori Partnership Boards) are not an add-on—we’re there to ensure our people are represented,” co-chair Hagen Tautari said.
The Board’s message is clear: honour Te Tiriti o Waitangi, or more Māori lives will be lost. The report calls on the government to trust whānau voices, back kaupapa Māori solutions, and meet their legal obligations under the Pae Ora Act.