Pae Ora Bill weakens Māori voice, erodes accountability
MEDIA STATEMENT
FOR IMMEDIATE RELEASE
Wednesday 4 March 2026, 4:00 PM
2 minutes to Read

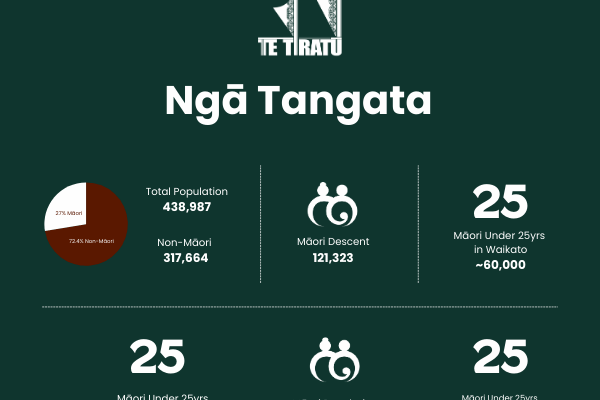
Te Tiratū Iwi Māori Partnership Board, representing over 121,000 Māori in the greater Waikato region, warns that the Pae Ora (Healthy Futures) Amendment Bill threatens to sideline Māori authority and strip Te Tiriti protections from New Zealand’s health system.
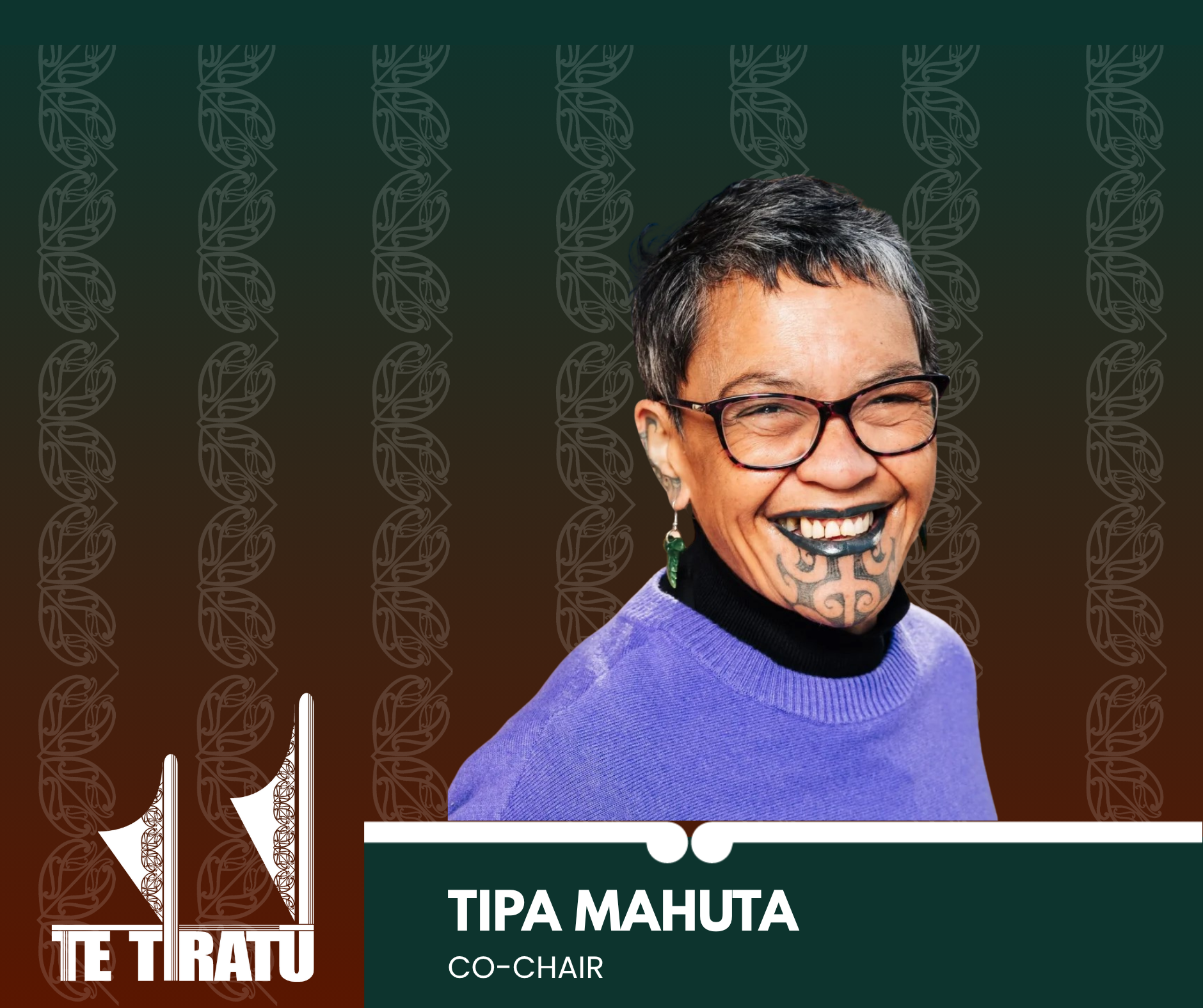
“This government talks about strengthening Māori voices, but these amendments sideline our authority. Iwi Māori Partnership Boards exist to ensure equity and accountability in health not just to provide advice when convenient. We need genuine power, not paper pathways,” said Te Tiratū Co-Chair Tipa Mahuta.
Drawing on the value of locality evidence from its Community Health Plan, Hauora Māori Priorities Summary, and Monitoring Reports on Te Whatu Ora, Te Tiratū believes weakening Section 30 of the Act reduces Māori decision-making, strip Te Tiriti protections, and deepen existing health inequities leading to poorer health outcomes for whānau.
“Our reports clearly show that iwi-led solutions improve access, outcomes, and efficiency across health services. From chronic disease management to cancer screening, the evidence demonstrates that local, Māori-led planning works. Yet the proposed reforms ignore this capability entirely.”
During last night’s debate, Te Pāti Māori MP Hana Maipi-Clark representing the Hauraki-Waikato Māori electorate warned that the Bill removes Māori influence and accountability from health governance.
“Iwi Māori Partnership Boards represent the community voice and Māori-led structures that ensure equity and accountability in our health system and this bill removes their influence.”
“Clause six removes the duty to maintain systems capable of understanding mātauranga Māori, kaupapa Māori services, and cultural safety and clause 33 strips equity and Te Tiriti expertise from public health advisory structures, including the Iwi Māori Partnership Boards. This is not tidying up legislation; it is dismantling accountability.”
Green MP Hūhana Lyndon added that IMPBs were originally designed to co-steer the system alongside Te Aka Whai Ora Māori Health Authority and Te Whatu Ora, but the amendments push them into the “back seat”:
While Labour argued “Why is the Government scared of local health services having to turn up to an iwi board and explain why they are not achieving outcomes for Māori? That is community accountability.”
Te Tiratū Iwi Māori Partnership Board point to the power of locally-led Māori responses during COVID-19 that were faster and more effective than centralised approaches.
“Our work shows the same principle applies across ongoing health inequities: whānau-led, evidence-driven governance delivers results,” Mahuta said.
Te Tiratū emphasises that Māori economic development depends on healthy, supported whānau. Empowered IMPBs drive workforce development, innovation, and local health infrastructure investment, aligning with Government economic goals.
“IMPBs play a critical role in ensuring Māori voices and mātauranga Māori shape health decision-making. Te Tiratū’s monitoring and priority reports provide actionable insights that improve outcomes and deliver stronger returns on taxpayer investment,” Mahuta said.
“The Crown’s duty to partner with iwi under Te Tiriti o Waitangi is non-negotiable. Reducing the role of the IMPBs risks repeating decades of systemic failure and wasted resources.”
12-Month prescriptions risk widening Māori health inequities without safeguards
MEDIA STATEMENT
FOR IMMEDIATE RELEASE
Friday 30 January 2026, 4:00 PM
2 minutes to Read

Te Tiratū Iwi Māori Partnership Board is warning that the introduction of 12-month prescriptions from 1 February 2026 risks increasing under-care, delayed diagnosis, and medicine-related harm for Māori unless strong equity and safety safeguards are put in place.
While Te Tiratū supports efforts to reduce barriers for whānau, Te Tiratū Tumu Whakarae, Brandi Hudson says affordability and convenience alone do not guarantee safe or equitable access to medicines.
“From a Hauora Māori perspective, access to medicines is not a single transaction, it is a continuous pathway of care,” she said. “Any policy change must actively uphold Te Tiriti o Waitangi obligations of partnership, equity and active protection.”
“Partnership means Māori are involved in designing and governing medicines access pathways, not just consulted after decisions are made. Equity requires ensuring Māori have the same access to subsidised medications and support services as others, addressing barriers like transport or culturally appropriate information. Active protection involves monitoring outcomes for Māori and adjusting policy to prevent under-care or delayed treatment,” she said.
The legislative change will allow prescribers to issue prescriptions covering up to 12 months for some medicines, with dispensing continuing in maximum three-monthly periods. Controlled drugs are excluded.
Māori already face significant barriers to accessing medicines. Despite higher rates of chronic conditions such as diabetes, cardiovascular disease, and respiratory illness, Māori are overall less likely to access dispensed medicines than non-Māori.
In some cases, prescriptions are not collected at all due to cost, access, and system barriers. These inequities mean that extending prescription duration alone will not ensure medicines safely reach whānau who need them most.
Dr Leanne Te Karu, expert advisor to Te Tiratū and author of its Tauāki Tū Position Statement on this policy change, says it carries significant risk if implemented without explicit safeguards.
“Māori already experience lower rates of monitoring, fewer proactive clinical reviews, and later diagnosis of chronic and complex conditions,” she said.
“Reducing prescribing touchpoints risks further decreasing opportunities to detect deterioration, review side effects, adjust treatment, or optimise medicines.”
Dr Te Karu warns that assumptions about “clinical stability” may be unsafe in contexts where care is fragmented, monitoring is inconsistent, and social and economic pressures affect medicine use.
“Prescriber discretion and unconscious bias can shape who is deemed ‘stable’.”
“Longer prescription intervals may be framed as empowerment when they instead reflect system withdrawal or under-service. Community pharmacists play a vital role, but they cannot replace comprehensive clinical review and diagnostic reassessment.”
Te Tiratū is calling on the Crown to ensure the implementation of 12-month prescriptions strengthens rather than weakens safety and equity, including through:
• Mandatory, equity-focused monitoring, with prescribing rates disaggregated by ethnicity, rurality, deprivation, disability, and continuity of care
• Transparent reporting of adverse events, hospitalisations, medicine changes, and wastage
• Māori-led evaluation of safety, trust, communication, and cultural safety
• Clear national guidance on who is not clinically appropriate for 12-month prescriptions
• A Te Tiriti-aligned medicines optimisation strategy, grounded in Pae Ora and mātauranga Māori
“Extending prescription duration alone will not improve health outcomes for Māori,” says Brandi Hudson.
“For a small number of whānau, longer prescriptions may be appropriate but only within a broader, equity-led system of care. Without strong safeguards, this policy risks entrenching, rather than reducing, inequity.”

Policy changes to prescription medicines must not place Māori at higher risk of harm or delayed care.
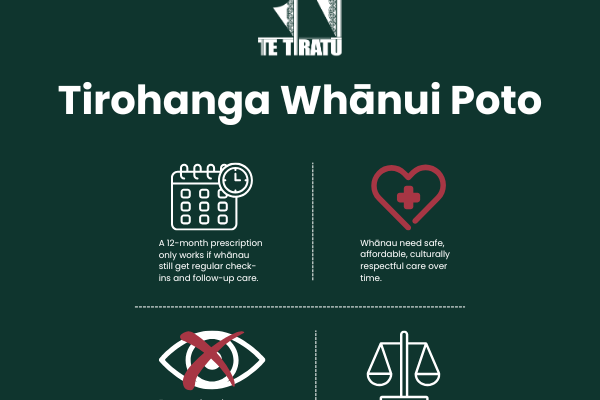
How this change to prescription medicine impacts our whānau from Tainui waka rohe.
New chair of Whānau Ora investment board across Upper North Island

From left to right (Front): Ernestine Walsh, (Chair) Dr Mataroria Lyndon, Riana Manuel, (Back) Leon Wijohn, (CE) Te Rōpu Poa, Dr Leanne Te Karu.
Te Tiratū Iwi Māori Partnership Board warmly congratulates Dr Mataroria Lyndon, on his appointment as Chair of the Rangitāmiro Whānau Ora Commissioning Agency Investment Board in a region of 2.3 million across the upper North Island.
“Rangitāmōro reflects the collective strength and vision of Te Tiratū Iwi Māori Partnership Board, Ngā Pou Hauora o Tāmaki Makaurau, and the National Hauora Coalition (NHC) who are tripartite partners,” said Glen Tupuhi, co-chair of Te Tiratū Iwi Māori Partnership Board.
“The leadership under Mataroria alongside that of his fellow board members gives us confidence that Rangitāmiro will advance what matters most to our people. The oranga and mana motuhake of whānau living in Te Tai Tokerau to Tūwharetoa, including Tāmaki Makaurau, Waikato and Hauraki.”
This critical leadership role places Dr Lyndon at the centre of strategic investment and assurance for Whānau Ora commissioning in the largest Whānau Ora region of Aotearoa.
Rangitāmiro is one of four newly contracted agencies operating under the Government’s Whānau Ora commissioning model.
The Investment Board is a structural safeguard to provide independent investment advice on how to best distribute funding to meet regional need. It will provide data‑informed direction on priorities, needs analysis, workforce planning and allocative frameworks all designed to strengthen confidence in investment decisions and outcomes.
“What makes this Board particularly significant is the breadth of expertise it brings from across whānau wellbeing, economic development, Hauora, social investment, commercial governance and Mātauranga Māori,” Dr Lyndon said.
“We will provide advice that directly informs commissioning priorities, regional needs analysis and workforce planning – key inputs for disciplined, evidence‑grounded decision‑making.”
The Investment Board’s membership reflects deep regional representation and technical expertise, and includes:
- Dr Mataroria Lyndon, Chairperson (Ngāti Hine, Ngāti Wai, Ngāti Whātua, Waikato‑Tainui)
- Riana Manuel (Ngāti Pūkenga, Ngāti Maru, Ngāti Kahungunu, Ngāti Whanaunga)
- Leon Wijohn (Ngāpuhi, Te Rarawa, Ngāi Tūhoe, Ngāti Tahu‑Ngāti Whaoa)
- Dr Tristram Ingham, KSO, MNZM (Ngāti Kahungunu, Ngāti Porou)
- Ernestynne Walsh (Ngāti Porou,Te Whānau‑a‑Apanui)
- Dr Leanne Te Karu (Ngāti Rangi, Te Ati Haunui-a-Pāpārangi, Muaūpoko)
The Investment Board sets investment priorities that are informed by whānau aspirations and evidence and guides allocative frameworks across the region to maximise both impact and equit
The Board provides strategic advice on a wide range of planning and investment activities, including the three-year Regional Needs Analysis, Investment Plans, and Regional Workforce Plans, while monitoring impact and performance to ensure that public investment delivers real value for whānau and communities.
Rangitāmōro has already contracted 301 kaimahi, including 120 new roles, to meet growing needs across its rohe from Tuwharetoa to the Far North, supported by a Government‑signalled Whānau Ora funding envelope of up to NZ$66,552,000 million per year for region 1 in 2025/26 and beyond.
Dr Lyndon brings significant governance and commercial experience to the role across health, research and governance sectors. He serves on multiple boards, including Rangitāmiro, and Te Tira Tū Iwi Māori Partnership Board, co-founding Tend Health, lecturing at the University of Auckland, and advocating for cultural safety to improve health outcomes, holding degrees from Harvard and Auckland.
His leadership underscores the commitment of Rangitāmiro to rigorous investment planning and assurance processes, in line with TPK’s commissioning model and expectations of arm’s‑length independence.
Some gains, many gaps remain for Māori health - System monitoring report
MEDIA STATEMENT
FOR IMMEDIATE RELEASE
Wednesday 3 December 2025, 9:00 AM
2 minutes to Read
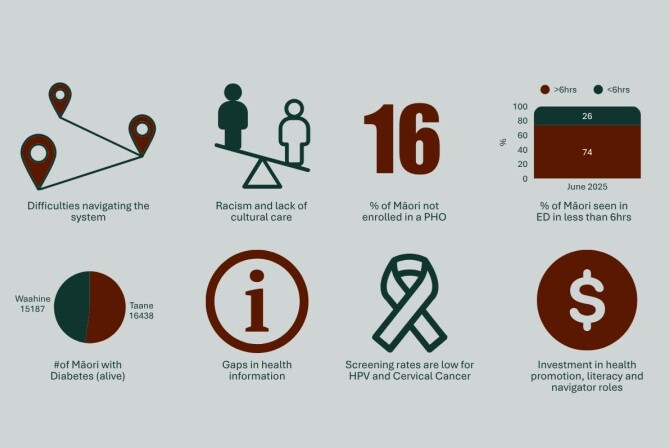
Te Tiratū Iwi Māori Partnership Board has released its latest Quarterly Monitoring Report, the second this year reviewing health system performance across the Tainui waka rohe in Waikato.
It builds on its inaugural report from June 2025 representing the interests of 121,000 whānau. While cervical screening rates have improved by 10%, ongoing inequities continue to affect whānau across the rohe.
“Since our first report, there have been small gains in areas like cancer treatment timeliness, but for too many whānau, the health system is still failing,” says Co-Chair Glen Tupuhi of one of the largest of the 15 Iwi Māori Partnership Boards established under the Pae Ora (Healthy Futures) Act.
“We are seeing Māori children fully immunised at just 60.8% far below the 95% target. Emergency department waits remain long, elective surgery delays continue, and access to primary care, especially in rural areas, is a major barrier.”
The report draws on lived experience from Whānau Voice surveys, limited Te Whatu Ora Health New Zealand data, and legislative benchmarks under the Pae Ora (Healthy Futures) Act 2022. Key findings include:
• Cancer treatment timeliness: 95.97% of Māori receive treatment within 31 days of diagnosis, slightly above the national target.
• Elective surgery: 31% of Māori wait more than four months for procedures.
“These numbers tell a clear story: inequity is entrenched and systemic barriers remain. Cost, distance, long wait times, and culturally unsafe services continue to harm whānau,” Tupuhi says.
The report also highlights ongoing gaps in Te Whatu Ora Health New Zealand’s reporting, governance, and partnership with iwi. Hauora Māori providers continue to deliver high-trust, culturally grounded services, but remain constrained by fragmented funding and siloed contracting.
Te Tiratū has shared the report with Te Whatu Ora and the Hauora Māori Advisory Committee, urging the findings to inform immediate action, investment, and policy reform.
“We’ve seen what’s possible when whānau are properly resourced and listened to,” Tupuhi says.
“Programs like Māori-led childhood immunisation show success, and now it’s time to scale that across all areas. Our goal remains a fair, accessible, and equitable health system one that honours Te Tiriti o Waitangi and the rights of our people.”
Background
Locality of Te Tiratū Iwi Māori Partnership Board represents the local Māori voice from:
1. Waikato – Central North Island, extending from the west coast (Raglan) inland to Hamilton and south towards Taupō.
2. Hauraki – Northern Waikato and the Coromandel Peninsula, bordering the Firth of Thames.
3. Maniapoto – Western-central North Island, covering the King Country, including Te Kūiti and Ōtorohanga.
4. Raukawa – South Waikato and central North Island, including Tokoroa, Putāruru, and Tirau.
5. Ngāti Hāua – Western-central North Island, around Taumarunui and the western Ruapehu district.
Rangatahi Māori mental health in rural Waikato is in crisis
MEDIA STATEMENT
FOR IMMEDIATE RELEASE
Tuesday 23 September 2025, 4:00 PM
2 minutes to Read

Despite the government’s ambitious July 2024 mental health and addiction targets, rangatahi Māori in rural Waikato are falling through the cracks. Te Whatu Ora Health New Zealand data with evidence from Te Tiratū Iwi Māori Partnership Board and local whānau voices shows that services are under-resourced, overstretched, and failing to meet the standards set by the government to monitor of health system performance by the Ministry.
National government targets include:
- Faster access to services: 80% of individuals to reach primary mental health and addiction services within one week, and mental health specialist services within three weeks.
- Emergency department efficiency: 95% of mental health-related ED presentations admitted, discharged, or transferred within six hours.
- Workforce development: Train 500 new mental health professionals annually.
- Prevention and early intervention: Allocate 25% of mental health funding to prevention.
Reality on the ground in rural Waikato:
- Over 200 tamariki/rangatahi have open referrals, with waitlists rising steadily since 2023 including 10 per month waiting for ADHD assessments and 21 for other mental health services.
- Frequent crises: Average of 10 crisis contact days per month, with 79 under-25s admitted to Henry Rongomai Bennett Centre since 2021 (average stay 14 days).
- Rural workforce gaps: Schools and providers rely on Police, St John, and Women’s Refuge to manage crises, far beyond their scope. Psychiatrists, psychologists, and counsellors are largely unavailable locally.
- Prevention funding gaps: Iwi- and whānau-led programmes like Hauora Waikato, Te Awhi Whānau, and Puāwai Project are underfunded despite proven success in building resilience and wellbeing.
“Our rangatahi are simply falling through the cracks,” says Brandi Hudson, Te Tumu Whakarae of Te Tiratū IMPB.
“The government has set clear targets, yet in rural Māori communities we are seeing long waits, repeated crises, and preventable hospitalisations. Immediate, targeted, and culturally grounded investment is not optional, it is urgent. I will be raising these issues directly with Minister Doocey when he visits Te Kūiti on Wednesday as part of his Rural Roadshow.”
Te Tiratū is calling on the government to prioritise early intervention and prevention for rural Māori youth, expand workforce capacity in King Country and other rural areas, fully resource iwi- and whānau-led programmes that are already proving effective, and ensure funding reaches the communities most at risk, not just metropolitan centres.
Without urgent action, the mental health crisis among rangatahi Māori will worsen, with devastating long-term consequences for whānau, communities, and the health system.
The Te Tiratū Iwi Maori Partnership Board represents the interests of 121,000 whānau Māori in the Tainui waka rohe and encompasses iwi from Waikato, Pare Hauraki, Raukawa, Te Nehenehenui (Maniapoto), Ngāti Hāua (Taumarunui), and Te Rūnanga o Kirikiriroa (Mātāwaka).
Minister Doocey will be at the Les Munro Centre in Te Kūiti for the Rural Roadshow from 12pm-1.30pm tomorrow.
Our strong warning that rangatahi Māori in rural Waikato are facing a mental health crisis.
Read the statistics Te Tiratū has gathered specifically for our Tainui waka rohe.
Glen Tupuhi appointed Co-Chair of Te Tiratū Iwi Māori Partnership Board
MEDIA STATEMENT
FOR IMMEDIATE RELEASE
Tuesday 23 September 2025, 9:00 AM
2 minutes to Read
Te Tiratū Iwi Māori Partnership Board (IMPB) representing 121,000 whānau across the Tainui waka region and one of the largest of the 15 Iwi Māori Partnership Boards established under the Pae Ora (Healthy Futures) Act is pleased to announce the appointment of Glen Tupuhi as Co-Chair.
He replaces Hagen Tautari, who has provided strong leadership and guidance governing to date. Tipa Mahuta, current Co-Chair, expressed her gratitude for Hagen’s service.
“On behalf of Te Tiratū IMPB, we sincerely thank Hagen Tautari for his dedication and commitment to the kaupapa, our whānau, and the wider Māori community. We are delighted to acknowledge Glen Tupuhi as our new Co-Chair and look forward to his leadership in guiding the Board forward,” she said.
From his time as chair of the Murihiku Māori Health Committee of the Southland Area Health Board in the mid 1980’s Glen brings over 35 years of governance experience across the Māori development, health, education, and justice sectors. His extensive background includes Iwi Hapuu Marae leadership roles as well as managerial roles in Oranga Tamariki, Corrections, Health Waikato, Hauora Waikato, and Te Rūnanga o Kirikiriroa. He has also served on the Auckland Council Independent Māori Statutory Board and the Māori Economic Development Panel.
Currently, he holds multiple governance roles, including:
- Independent Director, Winton Lands Ltd
- Board Member, Te Korowai Hauora o Hauraki and the Hauraki PHO
- Chair, Hauraki Localities Alliance
- Until recently Trustee of Ecoquest Education Foundation PTE and chair, Ngaa Muka Development Trust
A seasoned leader in integrating cultural perspectives with commercial decision-making, as chair of Ngaa Muka Glen has successfully guided iwi partnerships in projects across North Waikato such as Cobb Vantress chicken breeding plant, Lakeside development in Te Kauwhata and the initial establishment of the Sleepyhead Estate at Ohinewai, a $1.2 billion mixed-use industrial and residential development in North Waikato.
Glen’s iwi affiliations include Ngāti Pāoa ki Waiheke, Tamaki Makaurau, Hauraki, Waikato, Ngāti Hine, Ngāti Naho o Waikato, Ngāti Rangimahora, and Ngāti Apakura. His leadership philosophy emphasizes collaboration, strategic oversight, and creating sustainable opportunities for whānau and communities.
In addition to his professional and governance work, Glen continues to support whānau trusts and philanthropic initiatives, including the Whakatupu Aotearoa Foundation, fostering system-level change for communities and the environment in Aotearoa.
His appointment reflects Te Tiratū IMPB’s ongoing commitment to strong, culturally-informed governance, and the Board looks forward to the expertise, guidance, and leadership he will bring in advancing the aspirations of iwi and whānau across the region.
The Board encompasses iwi from:
- Waikato
- Pare Hauraki
- Raukawa
- Te Nehenehenui (Maniapoto)
- Ngāti Hāua (Taumarunui)
- Te Rūnanga o Kirikiriroa (Mātāwaka)
Proposed Pae Ora reforms lack evidence & crown’s Te Tiriti partnership with iwi non-negotiable
MEDIA STATEMENT
FOR IMMEDIATE RELEASE
Friday 1 September 2025, 8:00 AM
2 minutes to Read
Te Tiratū Iwi Māori Partnership Board (IMPB), representing over 121,000 Māori across the greater Waikato region, will present its submission opposing proposed changes to the Pae Ora (Healthy Futures) Act on Wednesday 3 September at 1.00pm.
One of fifteen Iwi-Māori Partnership Boards across Aotearoa, Te Tiratū stands united against proposed Pae Ora changes that would strip Te Tiriti protections, curb Māori decision-making, and deepen health inequities.
The Board warns that altering the roles and functions of IMPBs under Section 30 would undermine the Government’s commitments to Te Tiriti o Waitangi, equity, and meaningful Māori participation in health decision-making.
“Our leadership, knowledge, and influence are already delivering tangible results for whānau Māori,” said Co- Chair Tipa Mahuta. “The proposed reforms are not supported by evidence or Māori health data and risk reversing progress on improving outcomes for our communities.”
Te Tiratū highlights that IMPBs play a critical role in local and regional health planning, monitoring, and prioritisation, ensuring Māori voices and mātauranga Māori are central to decisions. Through initiatives such as the Community Health Plan and ongoing monitoring reports, IMPBs provide actionable insights to Health NZ and other agencies to drive better outcomes and stronger returns on taxpayer investment.
The Board points to decades of Māori-led success in health services, including the rapid and effective COVID-19 response, demonstrating that locally-led, iwi-driven solutions outperform traditional government approaches. Yet, Māori health inequities persist, with ongoing gaps in cancer screening, access to primary care, and chronic disease management. IMPBs are uniquely positioned to be the circuit-breaker to these long-standing disparities.
Te Tiratū also notes that the Government’s broader economic goals, including the “Going for Growth” Māori economic strategy, depend on healthy, supported whānau. IMPBs, if empowered, can drive innovation, workforce development, and local investment in health infrastructure, further supporting Māori economic growth.
“The Crown’s duty to partner with iwi under Te Tiriti o Waitangi is non-negotiable,” said Mahuta. “IMPBs must retain their legislated functions. Removing or diminishing our role risks repeating decades of systemic failure and wasted taxpayer resources.”
Te Tiratū urges the Minister of Health and Government to uphold Section 30 of the Pae Ora Act, ensuring IMPBs continue to lead, influence, and transform Māori health outcomes.
Third medical school must deliver for Māori – Te Tiratū welcomes $83M Waikato investment
MEDIA STATEMENT
FOR IMMEDIATE RELEASE
Friday 22 July 2025, 8:00 AM
2 minutes to Read

Image credit: Waikato Te Whare Wānanga o Waikato. An artist’s impression of the new Division of Health Precinct, which will be home to the New Zealand Graduate School of Medicine at the Hamilton campus.
Te Tiratū Iwi Māori Partnership Board representing 114,000 whānau Māori in Tainui waka rohe welcomes the Government’s announcement of $83 million in public funding, alongside philanthropic and university support, for the new Graduate School of Medicine at the University of Waikato Te Whare Wānanga o Waikato.
This investment marks a significant opportunity to address long-standing health inequities and workforce shortages in our region—especially for rural, Māori and underserved communities.
But this can only be realised if Māori health workforce development, cultural safety, and equity are embedded as foundational pillars in the new medical school’s design, training model, and governance.
“Whānau across Waikato have told us time and again: they want to see more Māori health professionals—people who understand our values, our lived experiences, and our ways of being as Māori,” said Tipa Mahuta co-chair of Te Tiratū Iwi Māori Partnership Board.
Māori currently make up less than 5% of the medical workforce, despite representing around 17–18% of the total population — a stark gap that highlights the urgent need for a more representative and equitable health system.
“Cultural safety is not a nice-to-have. It is essential to clinical excellence, trust, and good health outcomes. If patients don’t feel safe, they disengage—and that can cost lives,” Mahuta added.
The Te Tiratū Community Health Plan, Priorities Report, Monitoring Report, and Whānau Voice insights highlight critical barriers to care in the region:
- A lack of Māori-led service delivery options
- Inadequate rural and specialist services
- Persistent racism, judgement and cultural disconnection in some mainstream settings
Whānau are calling for a health system that is fair, accessible and reflective of the communities it serves. This means:
- A representative medical workforce that includes more Māori doctors, nurses, prescribers, dental/oral health professions, midwifes, therapists, mental health clinicians, sonographers, pharmacists, radiologists, anaesthetic technicians and specialists
- Clinical training of doctors grounded in kaupapa Māori values and culturally safe practice
- Data transparency and partnership with iwi and IMPBs in shaping workforce investment decisions
- Recognition of all hauora roles—from kaiawhina to clinicians—as part of a thriving Māori health ecosystem
As of 30 June 2025, there are 3,991 Māori registered with the Kia Ora Hauora the Māori health workforce development programme nationally. 240 identify with at least one iwi from Waikato. Yet many are still met with barriers, not bridges, into medical and health professions.
Te Tiratū urges the Government, Te Whatu Ora Health New Zealand, Hauora Māori Directorate and the University of Waikato to work closely with iwi, hapū and community partners to shape a graduate school that delivers on its promise—not only to grow the GP workforce of clinical placements across the country, but to heal a system given Māori die on average at least 7 years before non-Māori.
“We cannot miss this moment. A third medical school must reflect a third way—a culturally grounded, equity-driven, future-facing model of training that serves all New Zealanders, starting with those most underserved,” co-chair of Te Tiratū Iwi Māori Partnership Board, Hagen Tautari said.
Te Tiratū stands ready to partner and contribute to the new ‘Division of Health’ health precinct opening on the University of Waikato Te Whare Wānanga o Waikato campus.
The Board, under its statutory role in accordance with the Pae Ora Act, actively reflects and advocates for local Māori views on how public health services and public health initiatives are shaped and implemented.
The Board represents the whānau of Pare Hauraki, Waikato, Raukawa, Te Nehenehenui, Ngāti Hāua (Taumarunui) and Te Rūnanga o Kirikiriroa from the localities of Waikato, Hauraki, Maniapoto, Raukawa, Ngāti Hāua.

Kia Ora Hauora sees Waikato Tainui as a key strategic Iwi relationship within the Waikato region.

Programme Statistics – see overall Kia Ora Hauora statistics and statistics for Te Tiratū specifically.
Day one, same kaupapa: whānau ora thrives through Rangitāmiro
MEDIA STATEMENT
FOR IMMEDIATE RELEASE
Tuesday 1 July 2025, 6:00 AM
2 minutes to Read

The legacy of Dame Tariana Turia will continue to thrive under the new Whānau Ora Commissioning Agency, Rangitāmiro, for Te Tai Tokerau, Tāmaki Makaurau, Waikato, Hauraki and Tuwharetoa from today.
Rangitāmiro is a consortium of Te Tiratū Iwi Māori Partnership Board, National Hauora Coalition (NHC), and Ngaa Pou Hauora oo Taamaki Makaurau (Ngaa Pou Hauora).
Rangitāmiro Board Chair Eru Lyndon acknowledged the substantial responsibility of continuing Whānau Ora.
“The late Dame Tariana Turia led the remarkable legacy of Whānau Ora that encompasses the crucial journey of growing whānau capacity capability and independence. Dame Tariana was steadfastly focused on empowering whānau to reclaim authority of their situation, to determine the solutions that impact them and the generations to come. Starting today and continuing, Rangitāmiro is committed to Dame Tariana’s vision with heightened concentration and unwavering dedication to whānau.”
Rangitāmiro has the largest population of the four new commissioning agencies and board member Dr Rachel Brown said they’re operational.
“We’re building on the success of Whānau Ora commissioning agencies and the great work
that’s been done. They’ve benefited whānau – they’ve benefited my own whānau. The project team have been working tirelessly over the past few months on the transitional process with existing and new partners. We have contracted 301 new full time employees, an increase of 120 kaimahi allowing us to reach even more whānau than before with minimal disruption to meet the deep need from Tuwharetoa to the Far North. These are staggering results in a very constrained timeframe that shows our dedication to the kaupapa and allegiance to Whānau Ora.”
Board member Dr Mataroria Lyndon, who is also a Board member of Te Tiratū brings a wealth of knowledge to the Rangitāmiro board and he is confident the new commissioning agencies will help improve whānau outcomes across Aotearoa.
“I mihi to all of the new commissioning agencies who put their hands up to continue this extraordinary mahi delivering Whānau Ora support. It’s evident that, despite it being our first day, it’s not our first experience with this kaupapa. We’ve been working with whānau for decades, and we’re resolute in taking those values, alongside the powerful legacy of Dame Tariana, forward into the future for our respective regions. Dame Tariana had always spoken of the importance of mahitahi, whanaungatanga, and manaakitanga for Whānau Ora.”
Te Tiratū releases first “confronting” monitoring report on health system
MEDIA STATEMENT
FOR IMMEDIATE RELEASE
Friday 27 June 2025, 6:00 PM
2 minutes to Read
Te Tiratū Iwi Māori Partnership Board has released its inaugural Monitoring Report — a 46-page document under Section 30(1) of the Pae Ora Act 2022 that holds a mirror up to the system and asks two urgent questions: Is it working for us? And is it honouring Te Tiriti o Waitangi?
“This isn’t just data,” says Te Tiratū Co-Chair Tipa Mahuta. “It’s a reflection of what our whānau are actually living through every day — and it’s hurting them. The gap between policy promises and real-life outcomes is still too wide. Te Tiriti o Waitangi must be upheld in practice, it’s not a nice to do – it’s a must do.”
“Top of mind for our Board is the toll of cardiovascular, respiratory, and renal disease on our people which is simply devastating. Too many of our whānau are dying from preventable conditions — on average, seven years earlier than anyone else in the country.”
Representing 114,000 whānau across the Tainui waka rohe, Te Tiratū has drawn on lived experience from Whānau Voice surveying in the community, very limited data from Te Whatu Ora Health New Zealand, and legislative benchmarks to track system performance— and the findings are both sobering and clear – equity remains out of reach for too many Māori.
The report evaluates how well the system is delivering based on Te Tiratū’s regional health priorities, the five Government health targets, and Te Whatu Ora Health New Zealand’s statutory obligations under the Pae Ora (Healthy Futures) Act 2022.
It arrives at a pivotal time, as the Crown signals more major changes — including proposed amendments to Pae Ora after the disestablishment of Te Aka Whai Ora Māori Health Authority in its first 100 days.
“What we found in the report is confronting. Despite isolated gains — such as in mental health and addiction services — inequity remains entrenched. Our whānau continue to face multiple barriers to care, including cost, distance, culturally unsafe services, and long wait times,” said Mahuta.
Cancer screening rates for Māori remain far below national targets, and many Māori are missing out on essential primary care. Data is either missing or incomplete across key health areas like immunisation, oral health and long-term conditions — making it nearly impossible to track improvements or hold the system accountable.
The report also highlights that Te Whatu Ora Health New Zealand is falling short on many of its Pae Ora legislative obligations. Authentic iwi partnership in governance and decision-making is minimal or missing altogether.
Hauora Māori providers, while delivering high-trust, culturally grounded services, remain constrained by funding inequities and fragmented, siloed contracting systems.
Te Tiratū has sent the monitoring report to both Te Whatu Ora Health New Zealand and the Hauora Māori Advisory Committee and invited them to use the findings to shape advice to Minister Brown on investment, governance, and policy affecting Māori.
“We’ve seen what’s possible when whānau are listened to and resourced properly — particularly in areas like renewing the successful childhood immunisation programme run by Māori providers,” Mahuta said.
“Now we need to scale that success. We remain committed to advocating for a health system that is fair, accessible, and equitable — one that reflects the rights, needs and aspirations of our people.”