Hauora at home: Everything under one roof in Whaingāroa
Poihākena Marae in Whaingāroa Raglan was the place to be this week as whānau gathered hauora check-ups, hosted by Toi Oranga in partnership with a range of local and visiting health providers. The open-door event invited whānau to drop in, share a cuppa, and check up on their wellbeing — all in a familiar, friendly environment.
Nurses were onsite offering general health checks, alongside a wide range of services including physiotherapy, mirimiri (traditional Māori bodywork), immunisation, cervical screening, and counselling. A Ministry of Social Development (MSD) staff member was also available.
Two Heart Foundation representatives were kept busy with blood pressure checks, while a local GP provided full consultations in a dedicated clinical space.
Having services close to home made a big difference, particularly for kaumātua who often face challenges accessing care, and for younger whānau looking for convenient, supportive options.
“Whānau felt more comfortable at the marae, and not having to travel far — and having everything under one roof in such a friendly space just made sense,” said Megan Tunks, one of our Whānau Voice kaimahi.
Predominantly Māori came, but some non-Māori as well. “They relaxed with a hot drink and some kai, connected with others, and visited different service providers while they waited.”
Many of the visiting providers, including the physiotherapist and mirimiri practitioners, were from the local community themselves — a powerful reminder of the strength and value of community-led solutions.
The kaupapa was simple and effective: bring health services to where whanau already feel safe, respected, and connected. The result? A whānau-first day grounded in manaakitanga, kaitiakitanga, and whanaungatanga— showing what’s possible when hauora is delivered with aroha.
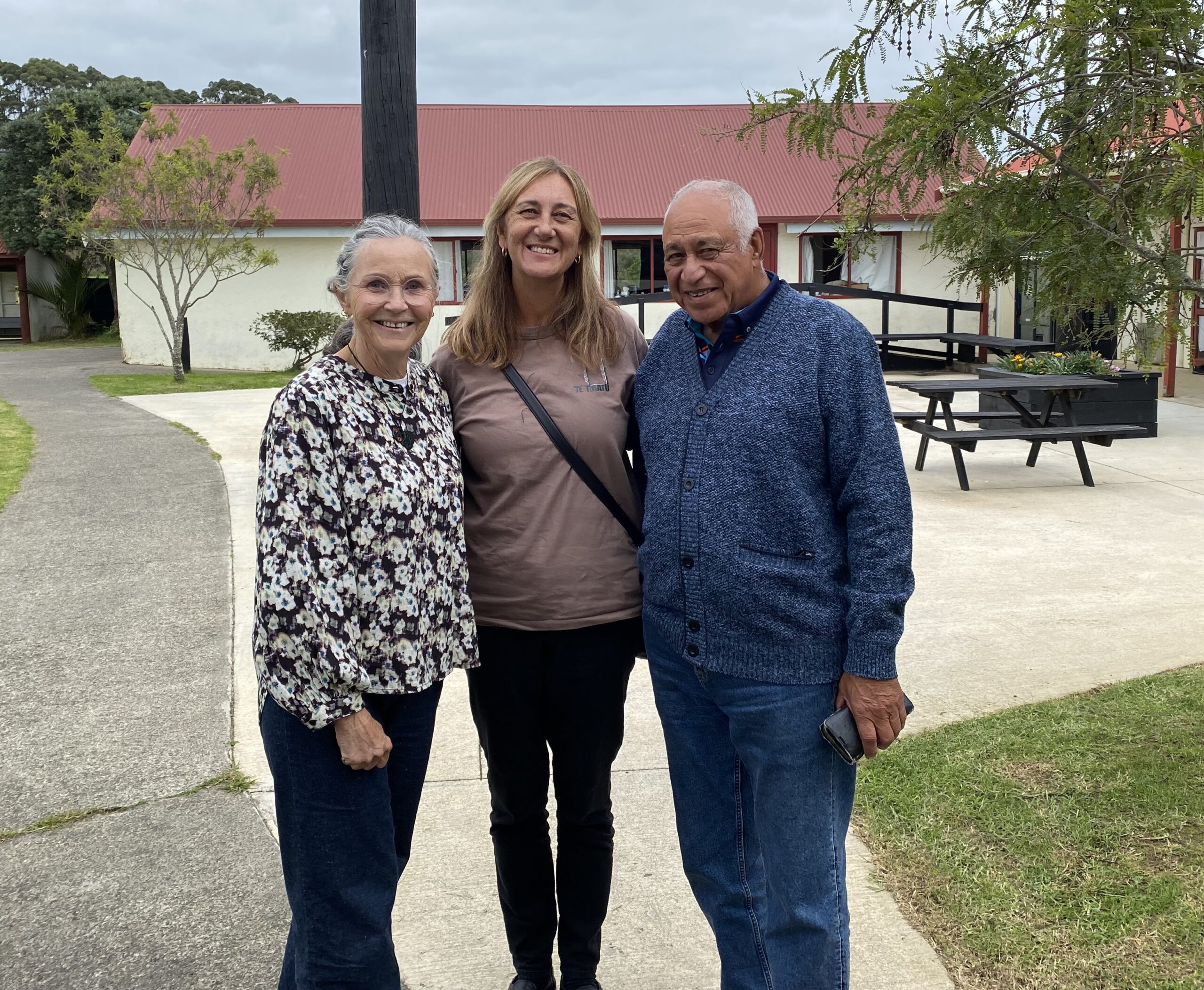
Photo: Lesley Thornley, a physiotherapist and daughter of the late Dr John “Digger” Penman, who served as the local GP from the 1940s to the late 1960s before being succeeded by Dr Ellison; Megan Tunks, Whānau Voice kaimahi with the Te Tiratū Iwi Māori Partnership Board; and Pablo Rickard, affectionately known as Whāingaroa Raglan’s ‘unofficial Mayor’.
From the Frontlines at Waahi Whaanui: Mental Health and Addiction Gaps
On the frontlines of whānau support, the cracks in the system are becoming impossible to ignore.
This week, our Whānau Voice team visited Waahi Whaanui in Raahui Pookeka-Huntly that was established in 1983 by the Tainui Maori Trust Board as one of its ten Marae Cluster Management Committees that works across a vast rohe — from Mercer in the north, to Raglan in the west, Te Hoe in the east, and Kirikiriroa in the south.
They deliver an impressive range of integrated services: Whānau Ora, parenting support, family violence response, social workers in schools, rangatahi transition services, alcohol and addiction support, and more. Deeply embedded in their hapori driven by a commitment to uplift whānau. But even with all their expertise, one reality stood out: they’re doing critical mahi with our people experiencing a health system under immense strain. The need is growing significantly, particularly for our rangatahi.
Mental Health: Access Denied by Distance and Delay
For Raahui Pookeka based whānau,often access mental health assessment is to travel half an hour to Hamilton. Once seen, they’re referred back to local services in Raahui Pookeka—services that are already under immense pressure.
The latest data from Te Hiringa Mahara – Mental Health and Wellbeing Commission backs this up:
- 16,000 fewer people were seen by specialist services in the year to June 2024, compared to 2021.
- More than 10,000 of them were under 25 years old.
- The drop isn’t because fewer people need help—it’s because they can’t get it.
This is a crisis. Not just of access, but of dignity.
Addiction Support Has a Waitlist—But Pain Doesn’t Wait
There’s a four-week wait to see an addiction counsellor at Waahi Whaanui. For some whānau, that’s a tipping point. There is limited alcohol and drug support for rangatahi under 18. We heard that many rangatahi are in crisis, with no place to turn.
Kaumātua Saving Up Their Pain
Kaumātua said they “save up” their health concerns because of cost and not wanting to be hōhā or overburden already stretched services.
It is not tika that they should feel like a burden. They carry our whakapapa, our mātauranga, our mauri. They should be cherished and prioritised.
The Numbers Are Stark—But Not New to Us
Māori in Waikato are:
- 9 times more likely than non-Māori to be hospitalised for any mental or substance use disorder
- 6 times more likely for schizophrenia
- 7 times more likely for substance and alcohol-related harm
- And an average of 225 Māori (mostly wāhine) are hospitalised for intentional self-harm each year
In Hamilton, over 2,000 Māori aren’t enrolled with a GP—shut out from the most basic preventative care.
Where to From Here?
What we saw was a failure of the health system to support providers like Waahi Whaanui who are under pressure, the increased caseload of kaimahi carrying too much without the resources they need, and whānau trying to hold on without falling through the cracks.
We stand alongside them—and we raise their voices.
Last week the Government announced a $28 million investment over four years in Budget 2025 to shift the response to 111 mental distress calls from Police to mental health professionals. For frontline providers like Waahi Whaanui it will take far more to address the deep gaps in accessibility, workforce, and culturally grounded care.
Te Tiratū is calling for:
Providers to be adequately resourced to cope with the increasing demand on services
- A focus on services for rangatahi under 18 that are locally relevant and accessible
- Appropriate whanau orientated triage processes
- Culturally grounded, local solutions led by whānau, hapū and iwi
Te Tiratū will continue to amplify your voice until the system listens.

From left to right: Rawinia Marsh – Integrated Services Manager Waahi Whaanui Trust, Fiona Helu and Hemi-Lee Morgan – Whānau Ora Team.
Maniapoto rising: “We know what works”
Our Whānau Voice kaimahi and Tumu Whakarae attended a recent hui held at Te Kūiti, hosted by Maniapoto Marae Pact Trust where a strong and heartfelt kōrero unfolded about the state of hauora for whānau across the Maniapoto rohe.
Frontline kaimahi, whānau navigators, and community leaders — including CEO Shirley Turner — came together to shine a light on what’s working, what whānau are asking for, and where the system is falling short.
“Our people know what works — we just need the system to back us,” Shirley said.
Maniapoto Marae Pact Trust offers a suite of integrated health and social services designed to walk alongside whānau, ensuring every door is the right door. These include:
- Kaiārahi Services – placing whānau at the centre, helping them define and lead their own goals across multiple service areas.
- Whānau Direct – offering fast, flexible support when whānau need it most.
- Disability support and mental health services, including social workers in schools.
- Tamariki Ora – a standout success story. The Tamariki Ora nurse and whānau navigator work together in the community, achieving strong immunisation rates despite not receiving equitable funding.

Photo from left to right: Te Tiratū Tumu Whakarae, Brandi Hudson with kaimahi of Maniapoto Marae Pact Trust – Sauaga Poliko, Lisa Kerekere, Rena Morgan, Honour Muraahi, Adrianna Astle and Raven Torea our Whānau Voice kaimahi
The Trust also contributes to Healthy Families Te Kūiti, with locals like Michelle Wi running weekly Māra Kai workshops on preserving, pickling, and food sovereignty — all part of a wider push for long-term wellbeing.
Shirley was clear about how the Trust works, “Whānau are in the driver’s seat — and that’s how it should be. Our services walk with them, not ahead of them.”
Systemic Challenges Undermining Equity
Despite these local strengths, systemic failures continue to undermine outcomes for Maniapoto whānau.
One striking example shared at the hui was of a kuia who was rushed by ambulance to Waikato Hospital with minimal belongings, only to be sent home later in a shuttle and left on the roadside.
It was only thanks to a member of the public contacting a local health worker that she made it home safely. This case highlights the urgent need for a more responsive, automatic travel support process — particularly around the National Travel Assistance (NTA) scheme.
“There needs to be a built-in, automatic system for whānau travel vouchers — not an afterthought.”
Other systemic concerns raised include:
- Falling through administrative cracks in post-hospital care and transport.
- No sustainable funding model for high-performing but underfunded services like Tamariki Ora.
- The need for better wellbeing measurement tools that reflect whānau realities.
- A desire for more regular, locally based specialist outreach, especially for kaumātua and kuia.
Networks and Ngā Kaupapa o te Rohe
The hui also acknowledged the strength of local collaborations — such as the Waitomo Community Health Forum and initiatives like Harvest to Home and Wai to Kai, which focus on food resilience, sovereignty, and wellbeing.
The message from Maniapoto is clear: local, kaupapa Māori solutions are working — but they need resourcing and system-level support.
“We’re seeing positive outcomes because our services reflect the lived reality of our whānau. But without equity in funding and process, our people continue to carry the cost,” said one kaimahi.
Calls for urgent action on dental equity
Coverage by The Waikato Local newspaper on the current situation in Taumaranui. Te Tiratū Iwi Māori Partnership Board (IMPB) listening to whānau has identified stark gaps in health access across the region—particularly in the areas of dental care.

Norton neighbourhood shares a few home truths
This weekend, in the heart of Norton, Hamilton, our Whānau Voices kaimahi joined a neighbourhood Hauora Event organised by the Wairiki Whānau Mentoring Trust, a Māori-led organisation dedicated to creating meaningful change for whānau living at the margins across the Waiariki and Waikato regions.
It provided a positive, safe and non-judgemental space where whānau could speak openly—free from stigma or blame. This environment allowed them to reconnect with their true selves, laying the foundation for healing and unlocking the potential for deep, transformational growth.
The gathering brought together whānau, local hapori, and the local MP, Tama Potaka. His presence highlighted the importance of connecting political leaders with the real experiences of whānau at the flax-roots willing to share their kōrero about the challenges they face within the health system.
Our Whānau Voice kaimahi were there specifically because Norton is a community marked by pockets of higher deprivation, often tied to long-standing inequities. These conditions create unique challenges for our people that need to be heard firsthand.
“They didn’t know who we were,” said Megan Tunks from Whānau Voice Te Tiratū Iwi Māori Partnership Board. “But we had more conversations in person with whānau, rather than relying on questionnaires.”
The stories shared revealed the harsh realities whānau face: “Whānau told us they’re waiting weeks just to see a GP—if they can afford it at all. Some are turning to A&E because urgent care is too expensive, and regular appointments are too short to get the help they need,” Megan said.

Photo: Waata Heathcote Chief Operating Officer Wairiki Whānau Mentoring Trust, Megan Tunks Whānau Voice kaimahi Te Tiratū Iwi Māori Partnership Board and the local MP, Tama Potaka.
One particularly poignant story was of a kaumātua who had suffered multiple strokes but was left waiting at a clinic with no clear support. “These stories speak to something deeper—it’s not just about access; it’s about trust and the way services engage with our whānau.”
For many, these struggles go beyond the healthcare system. “Our people aren’t just talking about barriers; they’re talking about survival—housing struggles, accessibility blocks, healthcare gaps, and the hopes they carry for their tamariki and mokopuna.”
Megan believes this feedback reveals a clear need for more mobile services that meet whānau where they are at. Hauora Māori services, she said, provide a safe and trusted space where whānau feel less judged and more understood.
This shift towards more accessible, mobile, and culturally supportive health services is vital for creating meaningful change in the lives of whānau.
Throughout the hui, common themes emerged around the need for culturally safe services, wraparound whānau support, and systems that honour te ao Māori ways of being.
These whakaaro are invaluable, and the voices captured will inform local priorities, service design, and future planning—ensuring that whānau are not just consulted but are co-creators of the solutions that impact their lives.
When whānau voices are elevated, transformation is not only possible, it is inevitable.
Ngā mihi nui to all who shared their time, courage, and whakaaro.
Turning whānau truths into system change - April 'whānau voice' report recap
At Te Tiratū Iwi Māori Partnership Board, our role under section 29 of the Pae Ora (Healthy Futures) Act 2022 is clear: to represent Māori voices—and to champion better health outcomes, better services, and better ways of working with the health system that reflect our realities, values, and aspirations.
Our April Whānau Voice Report lifts the lid on what’s happening in our homes, clinics, and hospitals—and what our whānau are calling for. We heard from 53 in our rohe, mostly Māori, mostly wāhine.
Behind every percentage and piece of data is a story—a lived experience of a whānau member trying to navigate a health system that too often feels cold, distant, and unaffordable.
“We’re still waiting.”
Too many whānau are waiting too long for care—GP appointments, referrals, or surgeries. Many whānau are living with multiple long-term illnesses—diabetes, cancer, heart disease—and are expected to manage complex conditions without enough support.
- 23% of respondents said the availability of healthcare is their biggest barrier.
- Many also shared that GP appointments are hard to get, and they often resort to visiting the hospital for non-urgent care.
One kuia shared how her husband finally had life-saving heart valve surgery—but no cardiac follow-up. “No specialist for his 6-week check-up—he wasn’t seen for 11 months. They found a growth and a tear around the valve.” She says they were lucky. What if they hadn’t pushed?
Whānau told us delays in accessing care—from GPs to surgery—are harming their health. “I’ve been waiting for gallbladder surgery since June 2023. It’s stopping me from going back to work.”
A mother said she’s been on the waitlist for her child’s ear operation for two years. Her tamariki has asthma, and their whare is cold. “Keeping the house warm is hard,” she said. “But we try.”
Another was battling on all fronts saying, “I’m dealing with diabetes, AFib, rheumatic fever, dementia, and a family history of cancer.” The lack of mental health services is not meeting the needs of whānau either —especially for tāne and tamariki.

Photo: Raven Torea Whānau Voice kaimahi Te Tiratū Iwi Māori Partnership Board and local whānau giving whakaaro.
“Not enough money.”
This is the silent crisis. Whānau are struggling to afford warm homes, healthy kai, and basic healthcare. For many, choosing between kai and medication is a painful daily decision.
- 27% of whānau said the cost of care is their biggest health barrier.
- That’s more than one in four.
The cost of living came up more than any other challenge. One father shared:
“I work seasonal jobs. I can’t always afford the doctor. So I wait.”
Another said: “Appointments, prescriptions, fuel to get there—it’s too much. Sometimes we choose between kai and meds.”
This is more than just money. It’s about dignity. About being forced to choose between filling a prescription or putting food on the table. About delaying care until it’s urgent.
“We go to the hospital because there’s nowhere else.”
When GP appointments aren’t available, hospitals fill the gap—especially for rural whānau.
- Many whānau told us they use ED services for non-emergencies.
- Others described long wait times, lack of transport, and stress.
Some said they waited from 8-11 hours at A&E—long, draining hours for kaumātua, pēpi, and māmā. Rural hospitals had shorter wait times 3-6 hours. Some had to give up and go home. Others sat in shuttle vans all day to reach the nearest hospital, with no breaks, no support, and no energy left.
“We’re rural,” one koro said. “It’s hard to get anywhere. The system wasn’t built for people like us.”

“We want doctors who understand us.”
Whānau told us they feel safer and heard when care is delivered by people who understand their world, their tikanga, their reo.
- 14% of respondents said the cultural safety of care needs to improve.
- Many said Māori health workers and services made a positive difference.
“We need more Māori nurses and doctors. They get us. They listen. They didn’t just treat us. They respected us.”
“When we went to a kaupapa Māori clinic, they treated us with mana. It wasn’t just the medicine—it was the whole experience.”
But too often, not everyone receives that experience and the opposite is true. One whānau shared a story about caring for their kaumātua in hospital: “The immigrant nurse lacked empathy. No pillow, no kindness, no empathy – it hurts.”
“We’ve got ideas, if someone would listen.”
Whānau didn’t just tell us what’s wrong—they told us what would help. Their priorities were consistent, clear, and backed by strong numbers:
- 24% of whānau said we need more doctors, more appointments, and shorter wait times. Our people are tired of waiting weeks—or months—to be seen.
- 27% said the cost of care is too high. Lower costs, especially for low-income families and those not eligible for subsidies, would make a huge difference.
- 14% called for better transport and services closer to home especially for rural and remotely based whānau, distance is a major barrier. More transport options and local services are needed.
- Another 14% asked for more culturally safe, Māori-led care—where whānau feel seen, heard, and respected.
- 13% want services that talk to each other, with better coordination and communication between providers, clinics, and hospitals.
- 10% reminded us that health doesn’t exist in isolation. They want whānau-centred, holistic support that includes safe housing, stable income, kai, education, and justice.
“Our care needs to reflect our world. Te ao Māori matters in healing.”
“It’s not just one thing—it’s everything.”
Whānau know what good care looks like. The system just needs to catch up.
These stories are not isolated—they are consistent, urgent, and reflect the reality that for many whānau, the health system is not delivering what it promised.
Te Tiratū carries a legal and moral responsibility to ensure our Whānau Voice reporting is heard. We will continue to advocate for a health system grounded in manaakitanga, equity, and tino rangatiratanga.
Building bridges with those who walk alongside whānau
Our Whānau Voice team had the privilege of visiting Kirikiriroa Family Services Trust in Kirikiriroa. This kaupapa has its roots in a unique tri-partnership between tripac partnership formed between Maatua Whāngai o Kirikiriroa, Specialist Education Services and Te Kōhao Health to provide the Family Start programme in Hamilton City.
Together, they built a service grounded in early intervention and strengths-based practice — empowering whānau to thrive in their communities by wrapping support around them when it’s needed most.
We were welcomed into their all-of-staff hui to kōrero about Te Tiratū — who we are, the mahi we do, and how Whānau Voice can be uplifted across the motu. We shared ways KFST kaimahi can participate in this kaupapa — as whānau themselves, and as advocates who walk alongside whānau every day.
The team at KFST were engaged and curious, especially around how insights are used to shape systems and services that work for whānau. Their openness signalled strong potential for future collaboration.

At its heart, our visit was about building bridges — whakawhanaungatanga between Te Tiratū Iwi Māori Partnership Board Whānau Voice kaimahi and those working in the community to strengthen whānau.
We know prevention starts with listening early and often. Our relationships with those who deliver frontline services to our Māmās, tamariki and rangatahi in particular are critical — especially those who may not be Māori-led but are deeply committed to whānau wellbeing.
By collaborating together, we ensure whānau are not only seen and heard, but that their voices carry influence — helping reshape the systems that impact their lives.
Ngā mihi nui ki te whānau o Kirikiriroa Family Services Trust. We look forward to continuing to walk this path together.
Bringing the smile back to Taumarunui: Dental care in the spotlight at Hapori Hauora Day
Crowds of whānau gathered today in Taumaranui at the Hapori Hauora Day, a health and wellbeing event designed to connect them with much-needed services—especially those that have been out of reach for too long, including oral health care.
Hosted at Taumarunui Hospital, the event organised by local and Te Whatu Ora services was supported by Te Tiratū Iwi Māori Partnership Board (IMPB) with its dedicated Whānau Voice kaimahi, and it drew attention to the stark gaps in health access across the region—particularly in the areas of dental, eye and ear care.
The Hauora Day provided on-the-spot services that included cardiac/diabetes/cancer screening, an eye clinic, immunisations, gall bladder/hernia/haemorrhoid banding specialists, to skin lesion clinics, but judging by the queues it was oral health and access to dental care that emerged as a top priority for many whānau attending.
“Parents expressed deep concern to get their tamariki seen—lining up in long queues to get access to the visiting dental teams. Yet the cost of treating their own dental issues remains out of reach. Many whānau do the best they can, using services when they’re available—but essential health care shouldn’t come down to waiting in line on a hauora day. That’s not equity—that’s survival,” said Brandi Hudson, Te Tumu Whakarae of Te Tiratū Iwi Māori Partnership Board.

A Call for Regular, Mobile Dental Services
Te Tiratū is advocating strongly for regular mobile dental services to visit remote and rural communities in South Waikato, where many whānau face significant barriers just getting to appointments—if they can find one. With few local dentists, high costs, and long travel times to urban centres, oral health has become a silent crisis.
Why Dental Matters
Oral health doesn’t exist in isolation. Poor dental care can lead to chronic infections, impact nutrition, self-confidence, and is closely linked to other health conditions like diabetes and heart disease. The Hapori Hauora Day included oral health education sessions, helping whānau understand these links and encouraging prevention. But education alone isn’t enough.
Pregnancy also increases the risk of dental issues, and with a high number of young Māori mothers and half the population under 25, the need for regular, accessible dental services is urgent and growing.
Looking Ahead: Growing a Māori Dental Workforce
The solution lies not just in service delivery—but in workforce development. Māori dental hygienists, therapists, and dentists are among the fastest-growing sectors in the health workforce, and the Te Tiratu wants to see that reflected in local service planning.
“Investing in our own people to deliver culturally grounded, community-based care is essential,” said Brandi Hudson. “And that starts with visibility. When our tamariki see Māori dentists in our communities, they start believing it’s a pathway for them too.”