'We cannot miss this moment': Waikato medical school must address health inequities - iwi
Te Tiratū Iwi Māori Partnership Board welcomes the Government’s $82.85 million investment in the new medical school at the University of Waikato, due to open in 2028 with an initial intake of 120 students.
Representing 114,000 whānau Māori in the region, Te Tiratū says this is a once-in-a-generation opportunity to tackle long-standing health inequities and workforce shortages—especially for rural, Māori and underserved communities.
Co-chair Tipa Mahuta emphasises that the school must embed Māori health workforce development, cultural safety, and equity from the ground up. “Cultural safety is not optional—it is essential for trust, clinical excellence, and better health outcomes.”
Co-chair Hagen Tautari adds, “A third medical school must reflect a culturally grounded, equity-driven model that serves those most in need.”
Te Tiratū stands ready to partner with Te Whatu Ora, Hauora Māori Directorate, the University of Waikato, iwi and hapū to shape a future-focused medical school that delivers for Māori.
Third medical school must deliver for Māori – Te Tiratū welcomes $83M Waikato investment
MEDIA STATEMENT
FOR IMMEDIATE RELEASE
Friday 22 July 2025, 8:00 AM
2 minutes to Read

Image credit: Waikato Te Whare Wānanga o Waikato. An artist’s impression of the new Division of Health Precinct, which will be home to the New Zealand Graduate School of Medicine at the Hamilton campus.
Te Tiratū Iwi Māori Partnership Board representing 114,000 whānau Māori in Tainui waka rohe welcomes the Government’s announcement of $83 million in public funding, alongside philanthropic and university support, for the new Graduate School of Medicine at the University of Waikato Te Whare Wānanga o Waikato.
This investment marks a significant opportunity to address long-standing health inequities and workforce shortages in our region—especially for rural, Māori and underserved communities.
But this can only be realised if Māori health workforce development, cultural safety, and equity are embedded as foundational pillars in the new medical school’s design, training model, and governance.
“Whānau across Waikato have told us time and again: they want to see more Māori health professionals—people who understand our values, our lived experiences, and our ways of being as Māori,” said Tipa Mahuta co-chair of Te Tiratū Iwi Māori Partnership Board.
Māori currently make up less than 5% of the medical workforce, despite representing around 17–18% of the total population — a stark gap that highlights the urgent need for a more representative and equitable health system.
“Cultural safety is not a nice-to-have. It is essential to clinical excellence, trust, and good health outcomes. If patients don’t feel safe, they disengage—and that can cost lives,” Mahuta added.
The Te Tiratū Community Health Plan, Priorities Report, Monitoring Report, and Whānau Voice insights highlight critical barriers to care in the region:
- A lack of Māori-led service delivery options
- Inadequate rural and specialist services
- Persistent racism, judgement and cultural disconnection in some mainstream settings
Whānau are calling for a health system that is fair, accessible and reflective of the communities it serves. This means:
- A representative medical workforce that includes more Māori doctors, nurses, prescribers, dental/oral health professions, midwifes, therapists, mental health clinicians, sonographers, pharmacists, radiologists, anaesthetic technicians and specialists
- Clinical training of doctors grounded in kaupapa Māori values and culturally safe practice
- Data transparency and partnership with iwi and IMPBs in shaping workforce investment decisions
- Recognition of all hauora roles—from kaiawhina to clinicians—as part of a thriving Māori health ecosystem
As of 30 June 2025, there are 3,991 Māori registered with the Kia Ora Hauora the Māori health workforce development programme nationally. 240 identify with at least one iwi from Waikato. Yet many are still met with barriers, not bridges, into medical and health professions.
Te Tiratū urges the Government, Te Whatu Ora Health New Zealand, Hauora Māori Directorate and the University of Waikato to work closely with iwi, hapū and community partners to shape a graduate school that delivers on its promise—not only to grow the GP workforce of clinical placements across the country, but to heal a system given Māori die on average at least 7 years before non-Māori.
“We cannot miss this moment. A third medical school must reflect a third way—a culturally grounded, equity-driven, future-facing model of training that serves all New Zealanders, starting with those most underserved,” co-chair of Te Tiratū Iwi Māori Partnership Board, Hagen Tautari said.
Te Tiratū stands ready to partner and contribute to the new ‘Division of Health’ health precinct opening on the University of Waikato Te Whare Wānanga o Waikato campus.
The Board, under its statutory role in accordance with the Pae Ora Act, actively reflects and advocates for local Māori views on how public health services and public health initiatives are shaped and implemented.
The Board represents the whānau of Pare Hauraki, Waikato, Raukawa, Te Nehenehenui, Ngāti Hāua (Taumarunui) and Te Rūnanga o Kirikiriroa from the localities of Waikato, Hauraki, Maniapoto, Raukawa, Ngāti Hāua.

Kia Ora Hauora sees Waikato Tainui as a key strategic Iwi relationship within the Waikato region.

Programme Statistics – see overall Kia Ora Hauora statistics and statistics for Te Tiratū specifically.
Rangatahi straight-up truths about hauora

Photo: Rangatahi Mokoia Hamiora-Houghton, the Kaitautoko/Kaitiaki of students from Rototuna High School attending the Kapa Haka and a Taiohi forum organised at Claudelands by Te Puna Wananga o Wairere.
Our rangatahi aren’t just open to kōrero—they’re confident, articulate and have important whakaaro that health leaders must listen too. In June, 96 chose to share their views through Whānau Voice surveys gathered both online and face-to-face. Combined with broader findings from our Community Health Plan, first Monitoring Report, and engagement activities between March and June, their voices offer powerful and direct insights into the health and wellbeing issues they care about most.
While many rangatahi were unfamiliar with some medical terms—particularly questions around the HPV vaccine—they showed curiosity and deep interest in learning more once questions were explained in plain language. What followed was a series of straight-up reflections that reveal the aspirations and challenges our young people face every day.
Mental health emerged as the number one concern. A third of all respondents saying they want more support and information in this space. Sexual health was another key area, especially among rangatahi worried about teen pregnancy and gaps in knowledge. Nutrition, the rising cost of healthy food, the dangers of vaping, and curiosity about rongoā Māori also featured strongly.
Here’s some of what they said:
- “Mental health & the dangers of vaping.”
- “As there’s so much teens who are hapū I feel like there needs to be more health info regarding sexual health and pregnancy.”
- “Nutrition info, particularly considering veggies and fruit are so expensive.”
- “More info about mirimiri in general would be awesome.”
What would help rangatahi stop – or not start – vaping? A lot of rangatahi told us they had tried vaping or were still vaping, even those as young as 12–17. They’re worried about how easy it is to access vapes, and many felt there should be tighter rules – like bans, stricter age checks, less advertising and more support.
Some of their whakaaro:
- “Ban vaping”
- “More restrictions, not advertising, and explaining the danger”
- “Need ID to purchase. There are places you don’t need it”
- “Give out methanol mints to encourage them to stop vaping”
Almost one in four said vaping should be banned or more tightly restricted. They also pointed to peer pressure as a key driver, and many said more mental health support and access to alternative activities—like sport, music, or creative outlets—would make a real difference.
“It’s the popularity of it, if mates do it others will too,” one rangatahi said.
Do rangatahi know about the HPV vaccine? Just over half had heard of the HPV (Human Papilloma Virus) vaccine. But nearly a third hadn’t, and some weren’t sure. It highlighted a mixed picture around the HPV vaccine. A significant number weren’t sure if they’d even been offered the vaccine at all, showing that school-based communication and consent processes may need strengthening. Even among those who had the vaccine, many still lacked clear understanding about what the vaccine is, why it’s important, or what it does in their bodies. This shows there’s still a big gap in the way health info is shared with our rangatahi – and it’s something we can work together to improve.
This kōrero with rangatahi reminds us that they are thoughtful, brave and full of ideas. When we take time to kōrero properly, they show up and are ready to lead, if we’re willing to listen. Their insights call for us—whānau, schools, health providers, and communities—to create safe space for deeper conversations and to ensure our health systems are reaching them with the right tools, messages, and manaakitanga. Our rangatahi have the answers. It’s time we act on them.
What’s really happening with cancer screening our rohe

Cancer impacts countless whānau across Waikato—and feedback from 23 whānau within the Tainui waka region, together with broader insights from our Community Health Plan, initial Monitoring Report, and engagement efforts from March to June, is revealing what’s effective, what’s falling short, and where services need to improve.
Our first Monitoring Report, released this month, shows that breast screening rates for wāhine Māori in Waikato continue to lag behind. Currently, just 54.5% of our wāhine are up to date with screening—7% lower than the national rate for non-Māori (64.6%). While there has been a small improvement of 1.1% since the last quarter, the pace of change remains too slow to close the equity gap.[1]
Most surveyed by our Whānau Voice team (nearly 74%) told us they regularly take part in cancer screening, particularly breast and cervical checks. Many said this is driven by personal or whānau experience of cancer. One participant shared: “My mum had cancer… I made self-referrals. I know how important it is to catch it early.”
But behind those statistics lies a more complex picture. Screening isn’t always comfortable. Over half of respondents said the process left them feeling whakamā, exposed, or in pain. Several described experiences that were rushed or poorly explained—leaving them uncertain, anxious, or unlikely to return. One woman shared: “Didn’t want to go back after last time—felt exposed.” Another added: “It was painful and no one explained anything.”
This discomfort was often made worse by a lack of cultural safety. Māori participants talked about mispronounced names, feeling spoken over, or being asked sensitive questions without privacy. “The lady at reception was white and made no effort to pronounce my Māori name,” said one. Others spoke of rushed appointments and the feeling that their experience wasn’t respected or mana-enhancing.
Not everyone receives timely results, either. Some whānau said they had to chase clinics for updates, while others described waiting months for treatment—even when a diagnosis had already been made. One respondent noted: “We waited 3–4 months, even with private insurance. Treatment took 6–9 months. Too long.”
The good news? Whānau know what would help.
They asked for more Māori doctors and support workers, better access to information, and culturally grounded care that includes warm, respectful service and more whānau-friendly settings—like marae, mobile clinics, or iwi spaces. Many called for free screening for kaumātua, flexible appointment times, and reminders by text or email, noting that these are not offered consistently.
Suggestions were practical and clear:
- “More Māori health professionals, please.”
- “Better-informed and pre-screening promotion.”
- “Use marae and iwi groups to get the message out.”
- “Have a Māori support person due to the medical language.”
A little over half of those surveyed also had a whānau member diagnosed with cancer in the last three years, and nearly half of them said they did not receive enough information about the treatment journey or support services.
There’s a clear call here—not just for more education and outreach, but for services that genuinely listen, respond, and hold space for whānau with care. As one whānau put it: “We need more manaaki-focused care. It makes all the difference.”
This kōrero reinforces the need for screening services that don’t just invite people in but hold them with dignity, understanding, and culturally safe support. Because early detection saves lives—but only if our people feel safe enough to walk through the door.
[1] Pg 13 Source: https://tetiratu.co.nz/wp-content/uploads/2025/07/2025-Te-Tiratu-IMPB-Monitoring-Report-to-March-2025.pdf
GP door closed for many: Whānau speak out

Photo: Kuia providing feedback at a recent Taumarunui Hapori Hauora Day
“We waited eight hours, and no one even told us how long it would be.”
This is the reality for many Māori whānau in the Waikato region, as shown in the latest Whānau Voice quarterly results that reveals the deep cracks in our primary care system.
These insights are drawn from a snapshot survey completed by 88 participants, alongside wider data gathered through our Community Health Plan, first Monitoring Report and engagement activities held between March and June. Their voices paint a clear picture judging by the indicative results, that our local health system is under immense pressure, and it’s pushing whānau to breaking point.
Despite more than 90% of respondents being enrolled with a regular GP, nearly 40% said they were unable to get an urgent appointment when they needed one. For many, the GP door feels effectively closed—whether due to fully booked clinics, high costs, or services being unavailable altogether.
In the first Health System Monitoring Report by Te Tiratū released this month, we note that key data from Te Whatu Ora is still missing. This includes:
- GP enrolment figures compared to the population (Māori vs non-Māori by age)
- Māori utilisation of GP services over the past 12, 24, and 36 months
- Māori utilisation by type of service (in-clinic vs virtual)
This lack of data limits our ability to assess equity in access and use of primary care services for Māori.[1]
So, in these moments of urgency, whānau are being forced to turn to urgent care clinics or hospital emergency departments for care that should be delivered by a GP. Nearly three-quarters of those surveyed said they had gone to A&E when they couldn’t get a GP appointment.
Of those, 29 percent reported waiting six to eight hours. Nine percent said they waited more than ten hours. Most waited without receiving any updates or basic information—86 percent received no health information during their wait, and 84 percent weren’t told how long the wait would be.
Adding to the strain, more than half of respondents said cost had stopped them or their whānau from getting care. This was particularly true for those in remote or rural areas like Tokoroa, Waharoa, and Huntly, where choices are limited and even getting to a clinic can be a challenge.
Some whānau reported being unable to enrol with a GP because no clinics were accepting new patients, or they lacked the required ID. These are not isolated stories; they reflect systemic barriers that need urgent attention.
What is Working?
Not all findings were bleak. Most people reported being able to get planned appointments when needed, and those who used telehealth services found them useful—90 percent said the advice met their needs.
Enrolment in a regular general practice remains high, which shows that there is a foundation to build from. But trust and consistency remain issues, with more than half saying they don’t get to see the same doctor each time.
This survey doesn’t just reveal long wait times or stretched services—it highlights the emotional weight of a system that too often leaves Māori whānau out of reach. It tells a story of people navigating closed doors, cost barriers, and uncertainty, just to access the care they deserve.
Te Tiratū Iwi Māori Partnership Board is using this data to advocate for urgent investment in services that are responsive, affordable, and culturally safe. Because no one should have to wait ten hours in an emergency room for care that should have been delivered in a clinic—least of all our tamariki and kaumātua.
[1] Pg 4 Source: https://tetiratu.co.nz/wp-content/uploads/2025/07/2025-Te-Tiratu-IMPB-Monitoring-Report-to-March-2025.pdf
It’s a confronting wake-up call
Photo: Te Tiratū Iwi Māori Partnership Board Co-chair Hagen Tautari
TVNZ’s Te Karere has aired a powerful segment on a new report from the Te Tiratū Iwi Māori Partnership Board, describing it as a “confronting wake-up call” for Aotearoa’s health system. The Board’s first-ever health system monitoring report reveals that Māori are still dying seven years earlier than non-Māori, with many of those deaths preventable.
The story highlights long waits, high costs, unsafe care, and poor screening rates as signs of a system that continues to fail Māori. “All of us, in particular with government, they need to ensure that the funding is adequate to protect our people,” said a Board representative. “We (Iwi Māori Partnership Boards) are not an add-on—we’re there to ensure our people are represented,” co-chair Hagen Tautari said.
The Board’s message is clear: honour Te Tiriti o Waitangi, or more Māori lives will be lost. The report calls on the government to trust whānau voices, back kaupapa Māori solutions, and meet their legal obligations under the Pae Ora Act.
From knowing to showing: Social value in focus at provider Forum

Photo: Te Tiratū Tumu Whakarae, Brandi Hudson (right) with Christine Arihia Brears (second right) and her kaimahi who travelled all the way from Taumarunui Kokiri Trust and Maniapoto Whanau Ora Centre to the Forum.
How do we truly shift the dial on health outcomes for whānau? For Te Tiratū Iwi Māori Partnership Board, the answer lies in listening to our providers, communities, whānau, aligning systems, and proving impact.
On Friday, over 30 kaimahi gathered at the Waikato Innovation Centre for Te Tiratū’s second Provider Forum, where Tumu Whakarae Brandi Hudson shared an update on kaupapa milestones before the rōpū moved into a wānanga on how data—can be a powerful tool for transformation, including a deeper kōrero on Social Return on Investment (SROI).
Two self-confessed, “old hands at this” Tammy Lehar and Susan Turner appreciated how space was created for partners who haven’t yet had the opportunity or experience, to come into a common kōrero together. “It’s something beautiful — if it’s done with the right intentions,” they said.
Tammy also highlighted the importance of building intentional data infrastructure “so we’re collectively working towards a shared vision—rather than duplicating efforts or collecting data in siloes.”
“We have the National Iwi Board Chairs Forum and the Iwi Māori Partnership Boards (IMPBs) with a common intention of strengthening data collection in this space. But to create meaningful connections between data and whānau outcomes, we must first build strong, integrated connections between these existing and emerging infrastructures—especially if we’re committed to a Whānau Ora approach.”
“This requires multiple, layered conversations. Personally, I’d challenge the assumption that Primary Health Organisations (PHOs) alone can provide a full picture, as they mainly reflect the primary health care lens. We also need to draw on data from other sectors, such as those funded under MSD and elsewhere, to understand the broader context of whānau wellbeing,” she said.
“There’s a foundational conversation needed—both at a local level and across the larger infrastructure. These discussions are already happening, but it takes time to bring the right people together in the right forum.” Innovation analyst Mari Tanioka from ImpactLab shared case studies on how to turn deep community knowledge into visible, trusted evidence.
“It’s a shift from knowing your mahi matters, to showing it clearly—using stories, numbers, and whānau voices. Often, what’s seen as anecdotal or informal is actually powerful insight. When made visible, it becomes a force for accountability and change,” she said.
Mari encouraged providers to start simple—by collecting clear, useful data such as how many whānau are being reached, or what barriers they face.
She gave the example of a provider who discovered, by tweaking just one survey question, that they were reaching over 63,000 tamariki—far more than they had previously realised. That kind of insight validates the mahi of kaimahi and helps funders better understand the scale and impact of their work.
The forum brought the philosophy of social investment into sharp focus. In a world of scarcity, complexity, and urgency, targeted support can change the course of a life. The difference between what a whānau’s future might look like without help—and what becomes possible with it—is what we call social value.
“Transforming lives through targeted interventions”— that, said Mari and her colleague Sarah Tuck, Engagement Manager at ImpactLab, is the heart of social investment.
Measuring that difference isn’t just about proving value—it’s about understanding what really works. Mari shared how one provider used SROI analysis to demonstrate that their slower, trust-based approach to health visits wasn’t inefficient—it was essential. With that evidence, they secured further funding.
Another organisation shifted strategy entirely, moving from diabetes treatment to prevention, after data showed how early engagement with whānau could help avert long-term harm.
For Te Tiratū, this mahi is about building strong, integrated systems that transform the system itself. Data alone is not the goal—it’s the pathway to transformation.
The shift from knowing to showing is more than a technical process. It takes time, care, and connection—but it’s what builds the momentum to reshape outcomes for our whānau, now and for generations to come.
Te Tiratū at the table of Rangitāmiro operating from Tūwharetoa to Te Tai Tokerau

Photo: Te Tiratū Tumu Whakarae, Brandi Hudson with Te Tiratū and Rangitāmiro Board member, Dr Mataroria Lyndon
Rangitāmiro is now fully operational, prepared to serve whānau across the largest region of all four new Whānau Ora Commissioning Agencies — stretching from the Far North to Tūwharetoa. This readiness is no accident. It reflects months of deliberate and intensive engagement, with more than 300 hui held with whānau and providers throughout Te Tai Tokerau, Tāmaki Makaurau, Waikato, Hauraki, and Tūwharetoa.
These conversations have shaped our approach and ensured that those already receiving Whānau Ora support will experience continuity, not disruption, during this transition.
Among those helping to lead this kaupapa is Dr Mataroria Lyndon (Ngāti Hine, Ngāti Wai, Ngāti Whātua, and Waikato) — a board member of both Te Tiratū Iwi Māori Partnership Board and Rangitāmiro. With deep whakapapa ties across the region and a lifetime of service to whānau health and Māori-led systems change, Dr Lyndon is confident that Rangitāmiro will continue to uplift whānau across Aotearoa.
From today, 301 Whānau Ora Navigators are on the ground through Rangitāmiro providers — reaching 100% of Rangitāmiro’s contracted target with Te Puni Kōkiri. This includes a net increase of 120 new kaimahi to meet the deep need across our rohe. These roles are not just numbers — they are trusted relationships, born from community, delivering support that reflects the real lives and aspirations of our whānau.
The Rangitāmiro commissioning model has also evolved. More pūtea will reach communities, where it is most needed. A stronger data system will help Rangitāmiro see what’s working, for whom, and why — improving outcomes and accountability. Direct relationships with providers will ensure transparency, responsiveness, and impact.
What remains unchanged is the unwavering focus of Rangitāmiro: whānau.
Whānau wellbeing. Whānau dreams. Whānau tino rangatiratanga.
A new dawn for whānau ora: Te Tiratū at the launch of Rangitāmiro
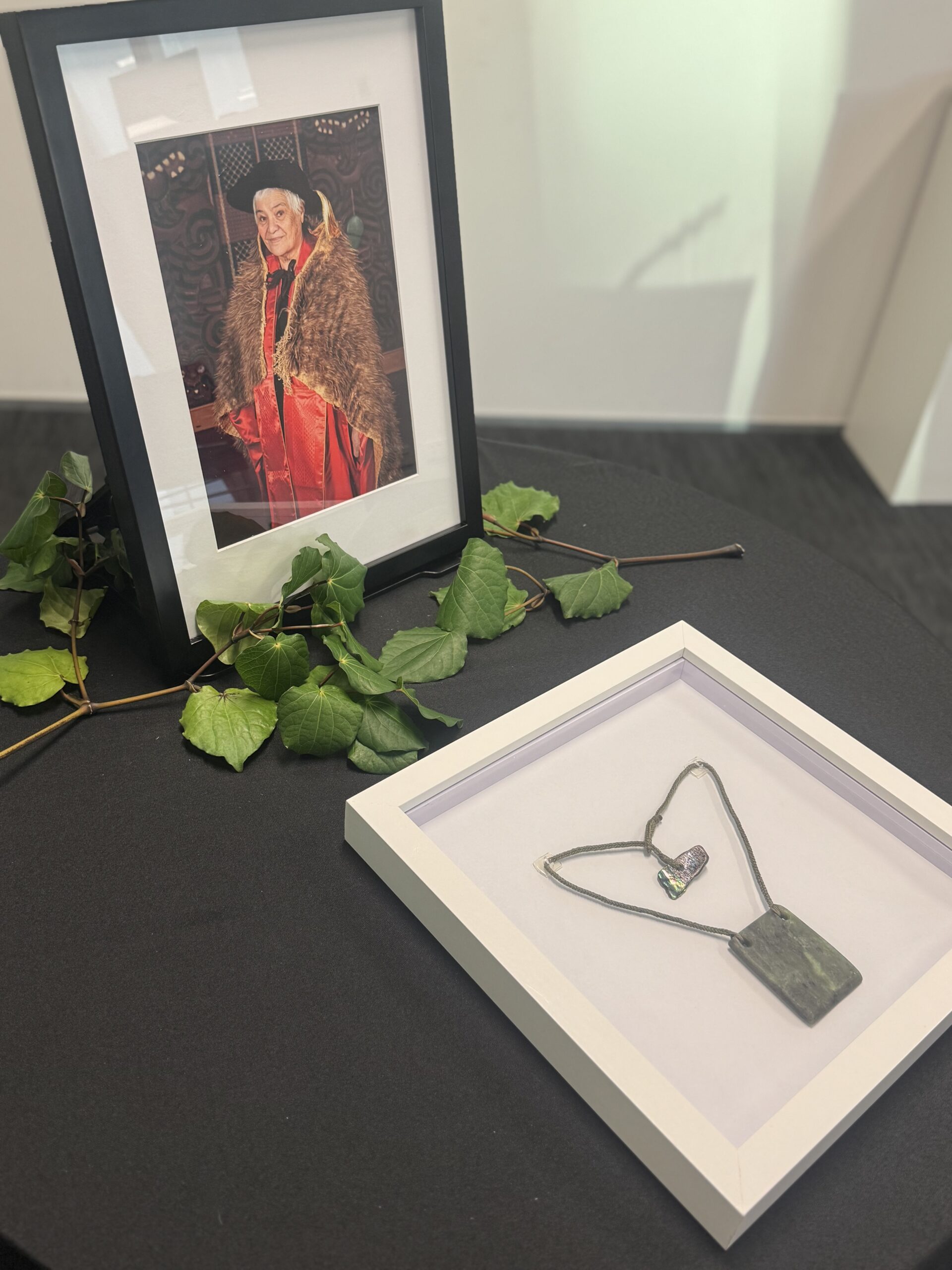
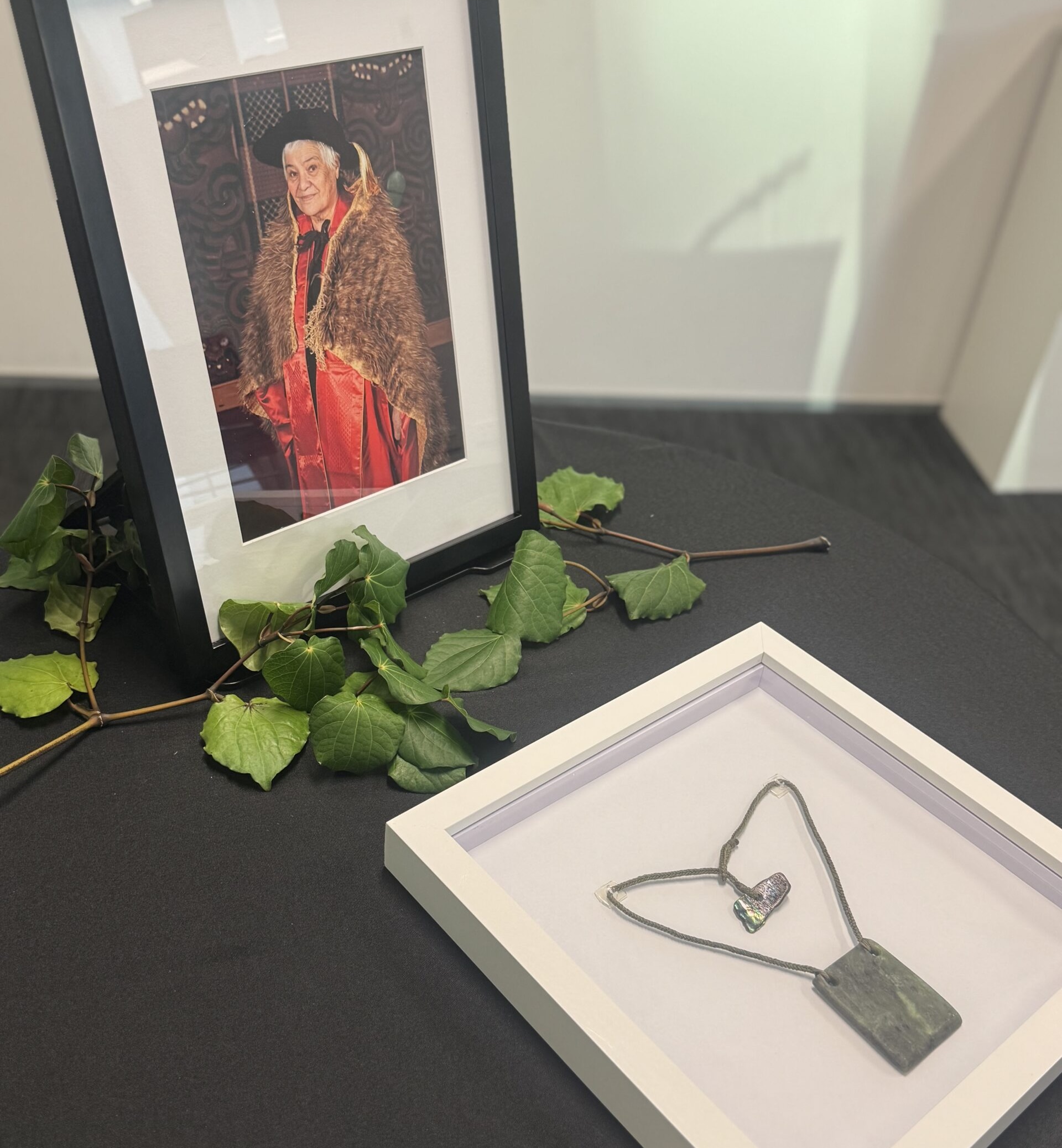
Photo: The late Kahurangi Tariana Turia and the mauri stone of Rangitāmiro
Early this morning, as the sun rose over Tāmaki, we gathered in karakia to mark the beginning of a powerful new chapter for Whānau Ora — Day One of Rangitāmiro, our new Whānau Ora Commissioning Agency for Te Tai Tokerau, Tāmaki Makaurau, Waikato, Hauraki and Tuwharetoa.
We carry forward the legacy of our beloved Kahurangi Dame Tariana Turia — with aroha, unity, and fierce determination. Her vision, rooted in manaakitanga, whanaungatanga, and tino rangatiratanga, continues to guide our mahi today. Whānau Ora is not just a policy; it’s a movement that centres whānau as the leaders and decision-makers of their own futures.
Rangitāmiro brings together the strength and vision of Te Tiratū Iwi Māori Partnership Board, Ngaa Pou Hauora oo Taamaki Makaurau, and the National Hauora Coalition (NHC). Together, we are focused on what matters most — the wellbeing and mana motuhake of our whānau.
Already operational, Rangitāmiro has contracted 301 kaimahi, including 120 new roles, to meet the growing needs of our region — from Tuwharetoa to the Far North. It holds the largest population of all four Commissioning Agencies and is committed to delivering services that support whānau across hauora, housing, kai security, oranga hinengaro, rongoā, financial wellbeing and more.
As a founding partner of Rangitāmiro, Te Tiratū stands proudly in our responsibility and honour to uphold Dame Tariana’s legacy. We were humbled to stand in karakia, to acknowledge our tūpuna, and to commit ourselves to this kaupapa once more — for our tamariki, our mokopuna, and all the generations to come.
“I mihi to all of the new commissioning agencies who put their hands up to continue this extraordinary mahi delivering Whānau Ora support. It’s evident that, despite it being our first day, it’s not our first experience with this kaupapa. We’ve been working with whānau for decades, and we’re resolute in taking those values, alongside the powerful legacy of Dame Tariana, forward into the future for our respective regions. Dame Tariana had always spoken of the importance of mahitahi, whanaungatanga, and manaakitanga for Whānau Ora,” Dr Mataroria Lyndon, Board member of both Te Tiratū Iwi Māori Partnership Board and Rangitāmiro.
Mā te huruhuru, ka rere te manu — with the right support, our people will soar.
Day one, same kaupapa: whānau ora thrives through Rangitāmiro
MEDIA STATEMENT
FOR IMMEDIATE RELEASE
Tuesday 1 July 2025, 6:00 AM
2 minutes to Read

The legacy of Dame Tariana Turia will continue to thrive under the new Whānau Ora Commissioning Agency, Rangitāmiro, for Te Tai Tokerau, Tāmaki Makaurau, Waikato, Hauraki and Tuwharetoa from today.
Rangitāmiro is a consortium of Te Tiratū Iwi Māori Partnership Board, National Hauora Coalition (NHC), and Ngaa Pou Hauora oo Taamaki Makaurau (Ngaa Pou Hauora).
Rangitāmiro Board Chair Eru Lyndon acknowledged the substantial responsibility of continuing Whānau Ora.
“The late Dame Tariana Turia led the remarkable legacy of Whānau Ora that encompasses the crucial journey of growing whānau capacity capability and independence. Dame Tariana was steadfastly focused on empowering whānau to reclaim authority of their situation, to determine the solutions that impact them and the generations to come. Starting today and continuing, Rangitāmiro is committed to Dame Tariana’s vision with heightened concentration and unwavering dedication to whānau.”
Rangitāmiro has the largest population of the four new commissioning agencies and board member Dr Rachel Brown said they’re operational.
“We’re building on the success of Whānau Ora commissioning agencies and the great work
that’s been done. They’ve benefited whānau – they’ve benefited my own whānau. The project team have been working tirelessly over the past few months on the transitional process with existing and new partners. We have contracted 301 new full time employees, an increase of 120 kaimahi allowing us to reach even more whānau than before with minimal disruption to meet the deep need from Tuwharetoa to the Far North. These are staggering results in a very constrained timeframe that shows our dedication to the kaupapa and allegiance to Whānau Ora.”
Board member Dr Mataroria Lyndon, who is also a Board member of Te Tiratū brings a wealth of knowledge to the Rangitāmiro board and he is confident the new commissioning agencies will help improve whānau outcomes across Aotearoa.
“I mihi to all of the new commissioning agencies who put their hands up to continue this extraordinary mahi delivering Whānau Ora support. It’s evident that, despite it being our first day, it’s not our first experience with this kaupapa. We’ve been working with whānau for decades, and we’re resolute in taking those values, alongside the powerful legacy of Dame Tariana, forward into the future for our respective regions. Dame Tariana had always spoken of the importance of mahitahi, whanaungatanga, and manaakitanga for Whānau Ora.”