Frontline voices on state of rural health in Thames
Associate Health Minister with responsibility for Rural Health, Matt Doocey and Minister for Rural Communities, Mark Patterson came to Thames today, to hear directly from the frontline about the challenges facing rural communities.
Doocey set out the five priorities of the Rural Health Strategy; recognising rural communities as a priority group, focusing on prevention for a healthier future, ensuring services are available closer to home, supporting access to services at a distance, and building a valued and flexible rural health workforce.
He also noted the review underway of the travel assistance programme, ongoing workforce pressures, and the rollout of one of six prototype digital telehealth services, with Thames chosen as a pilot site for 24/7 support.
While government priorities were outlined, much of the kōrero centred on the lived realities of staff, communities and a Māori provider of affordable health and wellness services across the Hauraki rohe for over 25 years.
Attendees described severe burnout among doctors and nurses, with calls for immediate workforce relief in Hauraki. Many emphasised that the bulk of the health workforce are women, yet parity in pay remains unresolved, creating inequity and undermining retention.
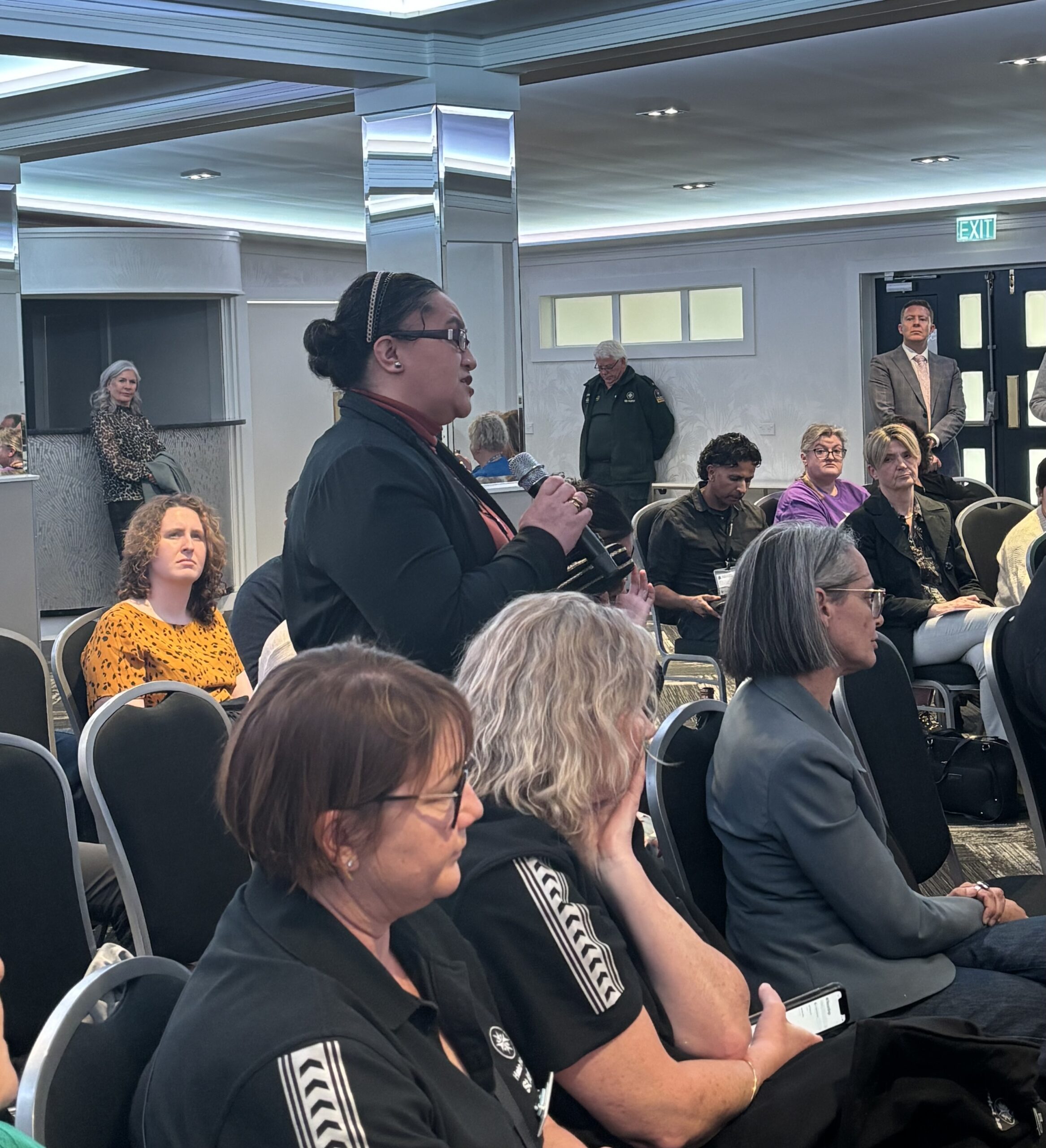
CEO of Te Korowai Hauora o Hauraki, Tammy Dehar, stood to share whakaaro about what integrated services might look like if they included the social determinants of health. She urged government to design solutions with communities rather than impose top-down targets, especially to support rangatahi. Similar calls were made for better training pathways, with regulated health body training and youth development identified as vital to the future of the rural health workforce.
Rural GP Alex McLeod also spoke out, saying good primary care services are not being given enough regard in government health design and resourcing. He said kaupapa Māori providers already deliver effective, whānau-focused care but are undermined by fragmentation and competition for funding. He urged government to consider local governance for primary care, rather than allowing secondary services to dominate leadership and decision-making.
In response, Doocey said immigration and skilled migration could help to address workforce shortages but were “not a silver bullet,” with policy settings needing to shift. He confirmed that a new mental health crisis response service is being developed with Police over the next three years and acknowledged the importance of building equity into workforce planning. A senior nurse and a nurse practitioner have also just been approved for the Thames Hospital ED.
Housing emerged as another barrier, with limited supply making it difficult for staff to stay and live locally. Safety was also raised, with communities dealing with domestic and sexual violence, drugs and alcohol, and the resulting rise in mental distress. Without adequate supports, attendees said, these pressures compound the crisis for both whānau and frontline services.
Transport and access challenges were highlighted, especially for elderly residents. After-hours services remain very limited. A short-term transport option provided by Thames Hospital earlier this year was welcomed but is not permanently funded. Seasonal pressures also weigh heavily, with the summer population in Coromandel surging from around 1,400 residents to 30,000 visitors, stretching an already fragile system.
In Waihi, residents face a three-day wait for telehealth services, with no permanent local health professionals and reliance on Thames Hospital ED. While Te Whatu Ora has committed to changes, attendees said stronger support for rural health practitioners is essential.
The hui also heard about local innovations such as the Colville Project, promoted and led by Dr Katie Armstrong, which integrates housing solutions, youth trainee pathways, and visiting specialist support. With $1.29 million already raised, the project demonstrates the ability of rural communities to design and deliver their own solutions when adequately supported.
The meeting showed that rural health cannot be transformed without resourcing the workforce, addressing housing and pay equity, and empowering local solutions that reflect the realities of rural communities. As Minister Doocey acknowledged, co-design and localism must sit at the heart of the Rural Health Strategy if it is to deliver for Hauraki and beyond.
Standing together for hauora – “Unity is what gives us mana”

Today, Te Tiratū Iwi Māori Partnership Board and Ngaa Pou Hauora oo Taamaki Makaurau Iwi Māori Partnership Board, representing over 210,000 whānau Māori, and partners in Rangitāmiro Whānau Ora Commissioning Agency gathered in Kirikiriroa for their first Board-to-Board hui to discuss the future of Māori health.
The kōrero focused on how the two IMPBs can work more closely together on hauora priorities and create future opportunities for Māori communities across Tainui waka rohe and Tāmaki Makaurau. One Board member reminded the rōpū, “The issues our whānau face don’t stop at regional boundaries. When we move together, our people are impossible to ignore.”
Legislative changes under the Pae Ora Bill and the statutory role of IMPBs were a major theme. There was strong consensus on charting an independent path forward that puts Māori voice and priorities at the centre of decision-making.
A key theme of the afternoon was mana motuhake, the power of designing health systems that reflect Māori realities. “We need to design systems for delivery that are inherently rooted in kaupapa Māori rather than being adjuncts to a system that was never built with the Māori experience of health in mind,” said one Board member. Another added, “We can’t wait for the system to decide what matters. We need to set the direction ourselves.”
The hui also highlighted the importance of joint advocacy and a stronger Māori voice. By working together with other Iwi Māori Partnership Boards, especially in high-population regions like Tāmaki Makaurau and Waikato, the collective scale of IMPBs strengthens national influence.
Aligning positions, sharing data, and producing joint communications ensures that both media and decision-makers cannot ignore the weight of Māori voices. As one participant noted, “Fragmentation weakens. Unity is what gives us mana.”
A significant discussion focused on how local priorities feed into national frameworks. Members explored the intersection between their Community Health Plans, the Hauora Ministerial Advisory Committee (HMAC), and the Government Policy Statement set by the Minister of Health.
As one board member explained, “Ideally, IMPBs set the final priorities through our Community Health Plans, HMAC puts those to the Minister, and those priorities become the Government’s priorities too.” This underscores the crucial role IMPBs play in ensuring whānau voices are not sidelined in policy and planning.
Both Boards also emphasised the need to move beyond deficit narratives. While inequities remain stark, the hui highlighted the importance of celebrating whānau successes and showcasing kaupapa Māori solutions already making a difference. “We are not just a story of struggle,” said one voice around the table. “We are innovators, we are resilient, and we already have answers that work.”
By the end of the hui, both Boards affirmed their commitment to Māori health priorities and keeping Whānau Voice at the centre. The message was clear, by staying strategic and united, the IMPBs will ensure Māori health priorities are carried strongly into national decision-making, with whānau voices shaping a system designed for them, not imposed upon them.
Institutions must turn the mirror – that’s where change begins
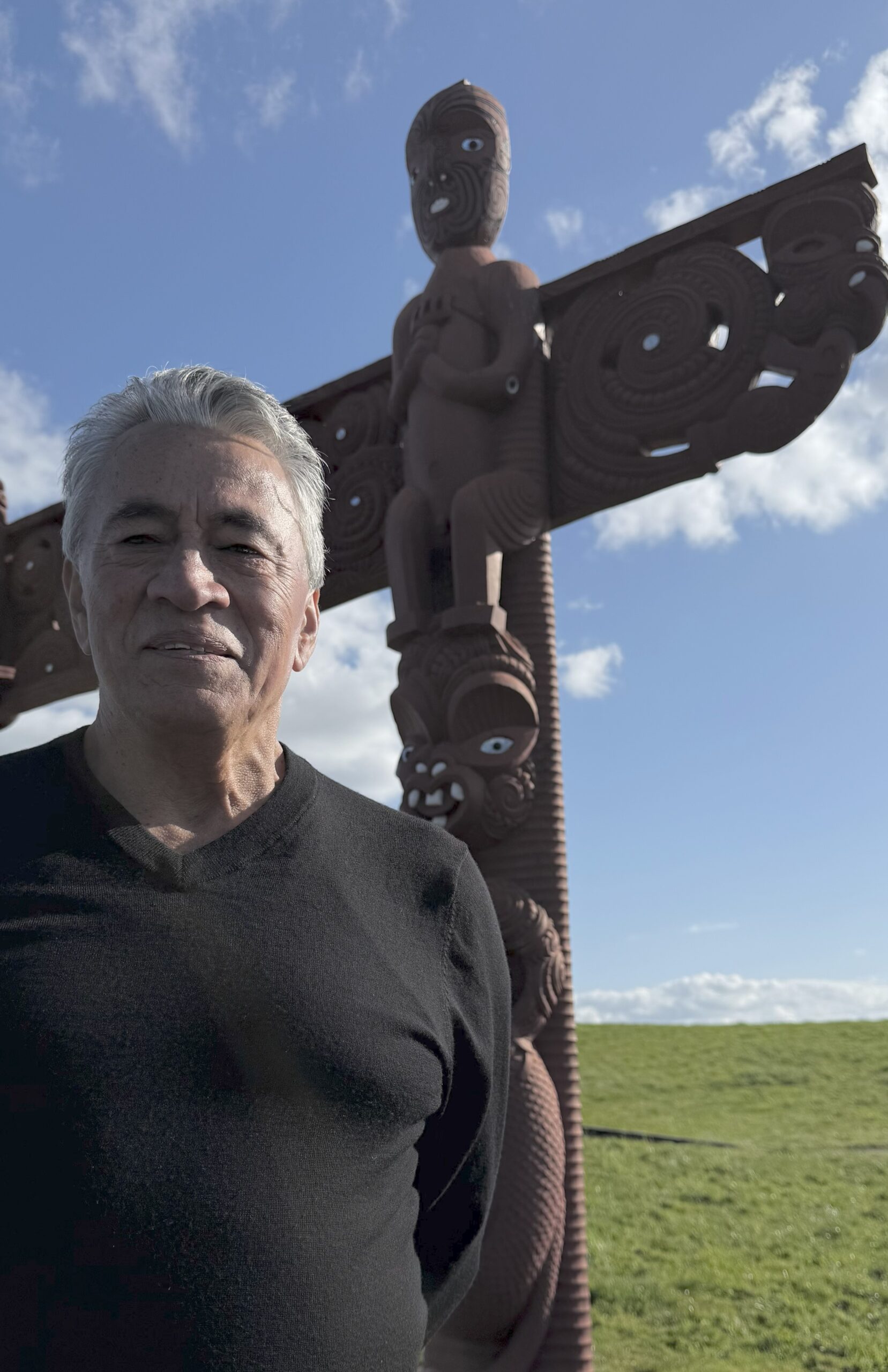
When Glen Tupuhi talks about governance, he doesn’t start with boardrooms or legislation. He starts with whānau.
In a recent radio interview with Ngā Iwi FM, he shared his vision as the new co-chair of Te Tiratū Iwi Māori Partnership Board. Known across Hauraki and beyond, Ngā Iwi FM is a trusted voice of iwi, hapū, and whānau in our Tainui waka rohe.
With more than 35 years of governance experience, Glen brings a deep understanding of leadership and accountability to his new role. For him, respect within the whānau and marae is the foundation for engaging rangatahi and building the next generation of leaders. His words of advice?
“Cut your teeth at the marae and whānau level. Our whānau are the most brilliant and the most challenging. If you can gain their respect, you’re unbeatable.”
Glen explained how the Waitangi Tribunal’s WAI 2575 inquiry shaped the Pae Ora Act, leading to the creation of Iwi Māori Partnership Boards like Te Tiratū, one of the largest across the motu.
“Most of our people are with mainstream services. For years, we’ve asked, if there’s inequity in health delivery to Māori, what is the responsibility of those services? The evidence before the Tribunal was irrefutable,” he said.
The Iwi Māori Partnership Boards under the legislation hold the health system accountable. But Glen says that monitoring role has been weakened with the proposal of the Pae Ora Bill currently before the Health Select Committee.
“We’ve ended up more like an advisory group. Meanwhile, doctors and nurses are powerful bodies in health, so what responsibility have they taken for the legacy of inequity? Everyone needs to step up.”
For Glen, becoming co-chair is a chance to carry the Hauraki voice into health governance trying to embed Māori voices and values into the heart of the system to get it back on the right path.
“On behalf of Hauraki, it’s a privilege to be here. David Taipari and I have always advocated strongly for the Hauraki voice, especially in health. Now we can strengthen that presence at the table,” he said.
He also sees rangatahi as central to the future of iwi leadership.
“I love hearing about rangatahi wānanga because they’re our forerunners. These are the spaces where they can spread their wings and build a great future.”
Glen draws on his years on the Waikato DHB Iwi Māori Council, where he saw the power of institutions taking responsibility for change.
“Instead of blaming Māori for not turning up to appointments, we asked, what is it about the way we deliver health that creates obstacles? It’s about turning the mirror on the institution. That’s where change begins.”
He believes mainstream health services need to adopt the same mindset, with clear measures to ensure equity.
“It’s not about us taking over. It’s about making sure people are delivering well to our whānau. Build equity into KPIs, audit them, and lift performance. That’s how we get real change.”
Call for urgent boost to rural Māori youth mental health services
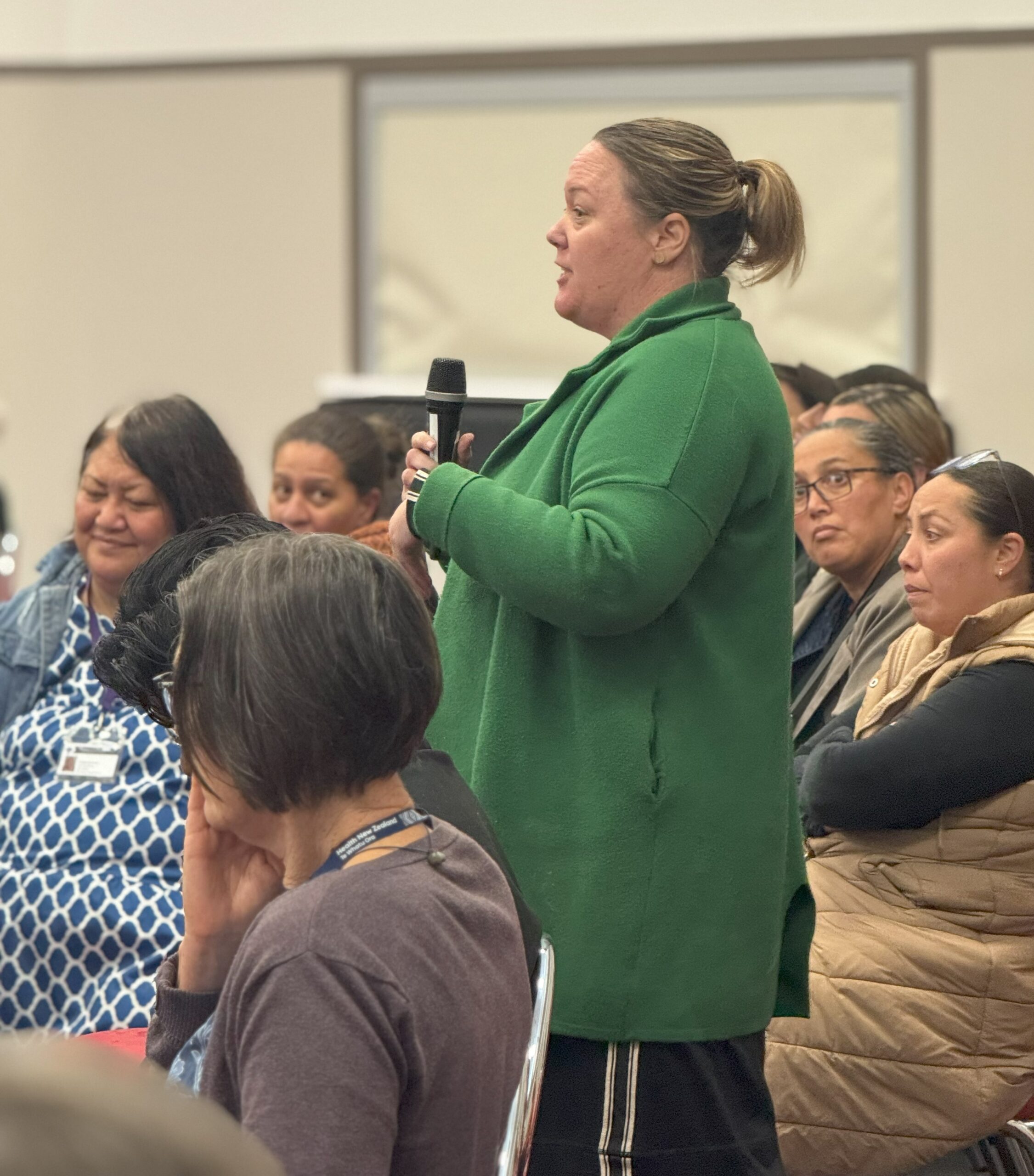
Brandi Hudson, Te Tumu Whakarae of the Te Tiratū Iwi Māori Partnership Board, is calling for urgent improvements to mental health services for rangatahi Māori, particularly in rural Waikato.
Speaking in an interview with Waatea News, Hudson says current funding and policy fail to meet the needs of Māori youth, with many rural whānau having to accept under-resourced services as normal. While initiatives like the Pou Wai Project and Hauora Waikato have shown success, they struggle to attract skilled staff and need more support to expand.
“There’s a real need for policy and investment that prioritises rurally based programmes designed and delivered by Māori, for Māori,” Hudson says, stressing that one-size-fits-all approaches won’t address the unique challenges of rural communities.
Rural Health Roadshow: Te Kūiti Speaks
Yesterday, the Les Munro Centre in Te Kūiti was packed as Te Tiratū Iwi Māori Partnership Board attended the Rural Roadshow. Mental Health Minister Matt Doocey and Minister for Rural Communities Mark Patterson listened as the community spoke directly about the real issues affecting them so both ministers and bureaucrats heard their voices firsthand.
Minister Doocey admitted that while national targets for health services may appear strong, performance in rural areas, particularly for rangatahi Māori mental health, lags significantly behind.
“Nationally we might be hitting 80 percent, but in rural Māori communities, the figures drop sharply,” he said. He praised the importance of local decision-making, stressing that community knowledge is essential to design effective services, and shared that the government is prioritising investment in underperforming areas, with $2.8 billion committed to mental health services this year, aiming to resource local providers and lift access and outcomes.
Key Questions from the Community
Local doctors, Kaimahi, and hauora Māori providers raised concerns that included access to care, noting that in some rural areas travel times to a hospital can exceed three hours, meaning urgent care is often delayed. Workforce shortages were another pressing issue, with providers asking what strategies will be implemented to retain doctors, nurses, and Māori health practitioners in rural areas. Digital health limitations also surfaced, with communities highlighting the challenges of telehealth in areas without reliable internet. Sustainable funding and integration of services were other priorities, with providers questioning why many community services still receive only one-year contracts and how mental health, primary care, social services, and housing can be coordinated locally.
Various locals raised the broader determinants of health, including alcohol accessibility, youth vaping, housing, and poverty, noting that these factors directly influence mental health outcomes. A story was shared about intergenerational trauma, the lingering impact of war, and how past experiences of discrimination and stigma continue to shape the mental health landscape for whanau living rurally and remotely in the rohe today.
Ministers’ Responses
Minister Doocey spoke about targeted investment to underperforming regions and the importance of enabling local providers to design solutions from the ground up. Relational commissioning was highlighted as a key approach, allowing communities to develop services that meet their own needs rather than relying solely on top-down directives. He spoke about ambitious mental health targets, including one-week access for primary mental health services and three-week access for specialist services, among the fastest internationally.
Ministers discussed workforce development as a critical piece of the solution, encouraging rural students to pursue healthcare careers and return to their communities. Initiatives such as mobile health screening units, and integrated care prototypes currently on the drawing board as innovative ways to improve equity and access. Ministers also recognised the importance of preventative and early intervention services, stressing that timely support is vital to prevent minor health issues from escalating into serious conditions.
The meeting underlined that improving rural health requires both cross-agency government support and local leadership.
“Health isn’t just about seeing a doctor. It’s about housing, food security, education, and the broader environment. The government can pull a few levers, but ultimately communities drive what works,” said Minister Doocey.
Glen Tupuhi appointed to Te Tiratū role
The National Business Review (NBR) reports that Glen Tupuhi has been named co-chair of Te Tiratū Iwi Māori Partnership Board, joining Tipa Mahuta and succeeding Hagen Tautari. Te Tiratū, one of 15 boards established under the Pae Ora Act, represents around 121,000 Māori whānau across the Tainui waka region and ensures Māori perspectives shape local health services.
Tupuhi brings over 30 years of experience in Māori development across health, education, and justice, with leadership roles at Oranga Tamariki, Health Waikato, Hauora Waikato, Corrections, and Te Rūnanga o Kirikiriroa. He also serves on multiple boards, including Winton Land, Te Korowai Hauora o Hauraki, and the Hauraki PHO, and has led key economic and development initiatives in North Waikato.
Affiliating with multiple iwi across Waikato and Tāmaki Makaurau, Tupuhi’s appointment underscores Te Tiratū’s commitment to strong, culturally informed governance. Co-chair Tipa Mahuta welcomed him, thanking Tautari for his service and expressing confidence in Tupuhi’s leadership.
Rangatahi Māori mental health in rural Waikato is in crisis
MEDIA STATEMENT
FOR IMMEDIATE RELEASE
Tuesday 23 September 2025, 4:00 PM
2 minutes to Read

Despite the government’s ambitious July 2024 mental health and addiction targets, rangatahi Māori in rural Waikato are falling through the cracks. Te Whatu Ora Health New Zealand data with evidence from Te Tiratū Iwi Māori Partnership Board and local whānau voices shows that services are under-resourced, overstretched, and failing to meet the standards set by the government to monitor of health system performance by the Ministry.
National government targets include:
- Faster access to services: 80% of individuals to reach primary mental health and addiction services within one week, and mental health specialist services within three weeks.
- Emergency department efficiency: 95% of mental health-related ED presentations admitted, discharged, or transferred within six hours.
- Workforce development: Train 500 new mental health professionals annually.
- Prevention and early intervention: Allocate 25% of mental health funding to prevention.
Reality on the ground in rural Waikato:
- Over 200 tamariki/rangatahi have open referrals, with waitlists rising steadily since 2023 including 10 per month waiting for ADHD assessments and 21 for other mental health services.
- Frequent crises: Average of 10 crisis contact days per month, with 79 under-25s admitted to Henry Rongomai Bennett Centre since 2021 (average stay 14 days).
- Rural workforce gaps: Schools and providers rely on Police, St John, and Women’s Refuge to manage crises, far beyond their scope. Psychiatrists, psychologists, and counsellors are largely unavailable locally.
- Prevention funding gaps: Iwi- and whānau-led programmes like Hauora Waikato, Te Awhi Whānau, and Puāwai Project are underfunded despite proven success in building resilience and wellbeing.
“Our rangatahi are simply falling through the cracks,” says Brandi Hudson, Te Tumu Whakarae of Te Tiratū IMPB.
“The government has set clear targets, yet in rural Māori communities we are seeing long waits, repeated crises, and preventable hospitalisations. Immediate, targeted, and culturally grounded investment is not optional, it is urgent. I will be raising these issues directly with Minister Doocey when he visits Te Kūiti on Wednesday as part of his Rural Roadshow.”
Te Tiratū is calling on the government to prioritise early intervention and prevention for rural Māori youth, expand workforce capacity in King Country and other rural areas, fully resource iwi- and whānau-led programmes that are already proving effective, and ensure funding reaches the communities most at risk, not just metropolitan centres.
Without urgent action, the mental health crisis among rangatahi Māori will worsen, with devastating long-term consequences for whānau, communities, and the health system.
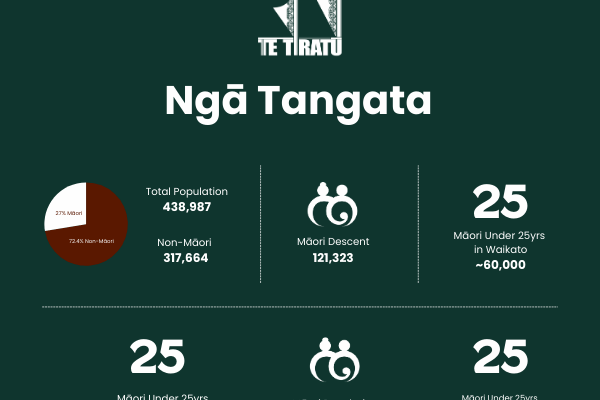
The Te Tiratū Iwi Maori Partnership Board represents the interests of 121,000 whānau Māori in the Tainui waka rohe and encompasses iwi from Waikato, Pare Hauraki, Raukawa, Te Nehenehenui (Maniapoto), Ngāti Hāua (Taumarunui), and Te Rūnanga o Kirikiriroa (Mātāwaka).
Minister Doocey will be at the Les Munro Centre in Te Kūiti for the Rural Roadshow from 12pm-1.30pm tomorrow.
Our strong warning that rangatahi Māori in rural Waikato are facing a mental health crisis.
Read the statistics Te Tiratū has gathered specifically for our Tainui waka rohe.
Glen Tupuhi appointed Co-Chair of Te Tiratū Iwi Māori Partnership Board
MEDIA STATEMENT
FOR IMMEDIATE RELEASE
Tuesday 23 September 2025, 9:00 AM
2 minutes to Read
Te Tiratū Iwi Māori Partnership Board (IMPB) representing 121,000 whānau across the Tainui waka region and one of the largest of the 15 Iwi Māori Partnership Boards established under the Pae Ora (Healthy Futures) Act is pleased to announce the appointment of Glen Tupuhi as Co-Chair.
He replaces Hagen Tautari, who has provided strong leadership and guidance governing to date. Tipa Mahuta, current Co-Chair, expressed her gratitude for Hagen’s service.
“On behalf of Te Tiratū IMPB, we sincerely thank Hagen Tautari for his dedication and commitment to the kaupapa, our whānau, and the wider Māori community. We are delighted to acknowledge Glen Tupuhi as our new Co-Chair and look forward to his leadership in guiding the Board forward,” she said.
From his time as chair of the Murihiku Māori Health Committee of the Southland Area Health Board in the mid 1980’s Glen brings over 35 years of governance experience across the Māori development, health, education, and justice sectors. His extensive background includes Iwi Hapuu Marae leadership roles as well as managerial roles in Oranga Tamariki, Corrections, Health Waikato, Hauora Waikato, and Te Rūnanga o Kirikiriroa. He has also served on the Auckland Council Independent Māori Statutory Board and the Māori Economic Development Panel.
Currently, he holds multiple governance roles, including:
- Independent Director, Winton Lands Ltd
- Board Member, Te Korowai Hauora o Hauraki and the Hauraki PHO
- Chair, Hauraki Localities Alliance
- Until recently Trustee of Ecoquest Education Foundation PTE and chair, Ngaa Muka Development Trust
A seasoned leader in integrating cultural perspectives with commercial decision-making, as chair of Ngaa Muka Glen has successfully guided iwi partnerships in projects across North Waikato such as Cobb Vantress chicken breeding plant, Lakeside development in Te Kauwhata and the initial establishment of the Sleepyhead Estate at Ohinewai, a $1.2 billion mixed-use industrial and residential development in North Waikato.
Glen’s iwi affiliations include Ngāti Pāoa ki Waiheke, Tamaki Makaurau, Hauraki, Waikato, Ngāti Hine, Ngāti Naho o Waikato, Ngāti Rangimahora, and Ngāti Apakura. His leadership philosophy emphasizes collaboration, strategic oversight, and creating sustainable opportunities for whānau and communities.
In addition to his professional and governance work, Glen continues to support whānau trusts and philanthropic initiatives, including the Whakatupu Aotearoa Foundation, fostering system-level change for communities and the environment in Aotearoa.
His appointment reflects Te Tiratū IMPB’s ongoing commitment to strong, culturally-informed governance, and the Board looks forward to the expertise, guidance, and leadership he will bring in advancing the aspirations of iwi and whānau across the region.
The Board encompasses iwi from:
- Waikato
- Pare Hauraki
- Raukawa
- Te Nehenehenui (Maniapoto)
- Ngāti Hāua (Taumarunui)
- Te Rūnanga o Kirikiriroa (Mātāwaka)
On the ground in Piopio: Health access struggles exposed at Te Nehenehenui Hui-ā-Tau

Photo: Whānau Voice kaimahi Raven Torea with kaumātua at Te Nehenehenui Hui-a-Tau
Whānau from Te Kūiti, Taumarunui, and surrounding areas came together at the Te Nehenehenui Hui-a-Tau, held at Napinapi Marae in Te Mapara, Piopio, to share their experiences with local health services, highlighting both the strengths of providers and the pressing gaps in care.
The hui, held on a clear and sunny day, provided an opportunity for kaumātua and whānau to discuss their needs and challenges with our Whānau Voice team. They reported using a mix of mainstream health services, including GP clinics, hospitals, dentists, midwives, physiotherapists, and optometrists, alongside traditional rongoā practices such as kawakawa teas, mirimiri, and herbal remedies. For many, GPs are a last resort, accessed only when traditional methods are insufficient.
Despite these resources, whānau emphasised the need for expanded services. Requests for more GPs, dentists, Māori-led health providers, mental health and counselling support, dieticians, and specialist services were consistent. Many whānau continue to travel to Waikato for care, often relying on friends or shuttles for transport, adding additional strain for elderly community members.
Access challenges were a recurring theme. Long wait times for GP and specialist appointments, lack of after-hours care, high costs for dental and optometry services, and limited information about available services all create barriers. Some whānau reported preferring to travel to Hamilton for glasses or dental care due to affordability and better service, highlighting inequities in local provision.
Despite these challenges, trusted providers received strong praise. Dr Rose Harris of the Maniapoto Whānau Ora Centre, which is part of the Taumarunui Community Kokiri Trust in Te Kūiti was highlighted as a Hauora Māori provider who delivers exceptional care, earning widespread respect from the community.
When asked about government health targets, whānau were unanimous in their assessment: the targets are not being met. “The government don’t see the struggles whānau have on the ground. They should walk in our shoes,” one wahine said. Another noted the higher rates of diabetes among Māori and Pasifika, adding, “No way. They’re not meeting them, and they need to go.”
Whānau also shared what supports their wellbeing. Engagement in marae and iwi activities, speaking te reo Māori, participating in physical activity, and spending time in nature were identified as key to maintaining health.
The hui underscored the importance of whānau voices in shaping health services. Whānau called for care that is accessible, culturally grounded, and delivered by Māori providers close to home. Their message was clear: health systems must meet the needs of the people they serve.
Proposed Pae Ora reforms lack evidence & crown’s Te Tiriti partnership with iwi non-negotiable
MEDIA STATEMENT
FOR IMMEDIATE RELEASE
Friday 1 September 2025, 8:00 AM
2 minutes to Read
Te Tiratū Iwi Māori Partnership Board (IMPB), representing over 121,000 Māori across the greater Waikato region, will present its submission opposing proposed changes to the Pae Ora (Healthy Futures) Act on Wednesday 3 September at 1.00pm.
One of fifteen Iwi-Māori Partnership Boards across Aotearoa, Te Tiratū stands united against proposed Pae Ora changes that would strip Te Tiriti protections, curb Māori decision-making, and deepen health inequities.
The Board warns that altering the roles and functions of IMPBs under Section 30 would undermine the Government’s commitments to Te Tiriti o Waitangi, equity, and meaningful Māori participation in health decision-making.
“Our leadership, knowledge, and influence are already delivering tangible results for whānau Māori,” said Co- Chair Tipa Mahuta. “The proposed reforms are not supported by evidence or Māori health data and risk reversing progress on improving outcomes for our communities.”
Te Tiratū highlights that IMPBs play a critical role in local and regional health planning, monitoring, and prioritisation, ensuring Māori voices and mātauranga Māori are central to decisions. Through initiatives such as the Community Health Plan and ongoing monitoring reports, IMPBs provide actionable insights to Health NZ and other agencies to drive better outcomes and stronger returns on taxpayer investment.
The Board points to decades of Māori-led success in health services, including the rapid and effective COVID-19 response, demonstrating that locally-led, iwi-driven solutions outperform traditional government approaches. Yet, Māori health inequities persist, with ongoing gaps in cancer screening, access to primary care, and chronic disease management. IMPBs are uniquely positioned to be the circuit-breaker to these long-standing disparities.
Te Tiratū also notes that the Government’s broader economic goals, including the “Going for Growth” Māori economic strategy, depend on healthy, supported whānau. IMPBs, if empowered, can drive innovation, workforce development, and local investment in health infrastructure, further supporting Māori economic growth.
“The Crown’s duty to partner with iwi under Te Tiriti o Waitangi is non-negotiable,” said Mahuta. “IMPBs must retain their legislated functions. Removing or diminishing our role risks repeating decades of systemic failure and wasted taxpayer resources.”
Te Tiratū urges the Minister of Health and Government to uphold Section 30 of the Pae Ora Act, ensuring IMPBs continue to lead, influence, and transform Māori health outcomes.