Rangatahi real talk at the Kapa Haka regionals

Photo: Rangatahi with Ngatini Torea and Raven Torea, Whānau Voice kaimahi
“We’re aware. We just need more support.”
That was the clear message from rangatahi and whānau who engaged with our Whānau Voice kaimahi at the inaugural Te Mokotini ki Tainui and Tainui Secondary School Kapa Haka regionals over the weekend. Alongside thousands gathered to celebrate te ao Māori, haka excellence, and hāpori, our Te Tiratū stand was part of a ‘Hauora Hub’ inside the doors of Claudelands Event Centre. The whare was humming with conversation — and concern. From rangatahi to kaumātua, whānau shared openly about their health journeys, what’s working, and what’s failing them.
What Our Rangatahi Are Saying
Across two days, rangatahi spoke frankly about what they’re facing. They’re switched on and vocal about the lack of mental health and sexual health education in schools — especially around hauora hinengaro. Many shared they learn more from social media than from the classroom. They know mental distress is a problem among their peers but feel unsupported by the current system. They want more—more kōrero, more guidance, and more honest talk in safe spaces. One rangatahi said it best: “We talk about it on TikTok, but not in class. That’s not right.”
Vaping: From “Cool” to “Can’t Stop”
We were alarmed by how widespread vaping is among rangatahi, particularly those aged 12 to 17. Nearly all told us they had easy access — either through shops not checking ID or older siblings buying on their behalf. What began as something “cool” quickly became something they couldn’t stop. Many now feel addicted. They want to quit, but said it’s hard — and support is scarce.
Their message was clear: restrictions aren’t enough. They believe a total ban is the only way to truly protect rangatahi. Importantly, they also called for earlier education, aimed at tamariki aged 10–12, before peer pressure kicks in and the dreaded addiction cycle begins.
Vaccination? Yes. Understanding It? Not So Much.
While most rangatahi had received their HPV vaccination at school, nearly none knew what it was for. One said: “I just signed the form. I didn’t even know what it was.”
This shows a huge gap in informed consent and health literacy. Our tamariki and rangatahi deserve to know what’s going into their tinana and why.
Primary Care: Cost, Wait Times & Whānau Avoiding Help
Whānau told us loud and clear: “If it’s not for the tamariki, we just don’t go.” The reasons are simple — long wait times and unaffordable costs. Standard GP visits range from $60 to $80, and after-hours care can be as high as $180. Many are turning to emergency departments by default, not because it’s ideal, but because it’s faster and more accessible. For some, the choice between paying rent or seeing a doctor isn’t really a choice — it’s about survival. While telehealth works for a few, unclear pricing has left others feeling misled — one whānau member was shocked when their father’s online consult cost more than an in-person visit.
Cancer Screening: Awareness Growing, But Gaps Remain
Many whānau had been screened for breast, cervical, or bowel cancer, but few had completed all three — and most had to initiate the process themselves, with little guidance from GPs or nurses. A registered nurse told us that while reminders appear in patient files, many health professionals simply overlook them. For wāhine, the screening experience was often described as cold and clinical, lacking cultural safety, with many feeling whakamā — exposed, undignified, and unlikely to return. There was positive feedback too, particularly around cervical screening reminders, which were clear and helpful, and the fast, reassuring turnaround times for breast screening results. However, follow-up care was inconsistent, and whānau made it clear they want more community-based education and engagement — they want to understand what to expect, why it matters, and how to access care before it becomes urgent.
Thank you For Your Truths
We’re deeply grateful to every whānau member and rangatahi who stopped by to share a laugh, a selfie, and a story — your voices are shaping the future of our hauora. Every kōrero is being carried forward in our regular reporting and meetings with Te Whatu Ora. We’re listening, and we thank you for trusting us with your truths.
Whānau Ora launches new agency with fresh leadership
Rangitāmiro, the Whānau Ora Commissioning Agency, has announced its inaugural board of directors and the appointment of its first chair. The collaborative includes Te Tiratū Iwi Māori Partnership Board with the National Hauora Coalition, and Ngaa Pou Hauora o Tāmaki Makaurau Iwi Māori Partnership Board.
Eru Lyndon (Ngāpuhi, Ngāti Hine, Ngāti Kahu, Ngāti Wai, Ngāti Whātua and Ngāti Toa) has been named chair of the board. Lyndon brings extensive governance experience, including being chair of Waitangi Limited and having board roles with the National Hauora Coalition, The Selwyn Foundation, and the University of Auckland Business School.
The appointed board members are:
- Dr Mataroria Lyndon (Ngāti Hine, Ngāti Wai, Ngāti Whātua, Waikato), member of Te Tiratū Iwi Māori Partnership Board
- Dr Rachel Brown (Te Ātiawa ki Wharekauri, Kāi Tahu), CEO of the National Hauora Coalition
- Shelley Katae (Te Rarawa, Ngāti Porou), Chief Executive of Tāmaki Regeneration
- Karen Wilson (Te Ākitai Waiohua, Ngāti Te Ata, Ngāti Pikiao), Chair of Te Ākitai Waiohua Settlement Trust
Rangitāmiro is part of a new commissioning model, Whānau Ora 2.0, which will be rolled out across four regions:
- Region 1: Rangitāmiro – Taupō to Northland
- Region 2: Te Rūnanga o Toa Rangatira – Wellington to Waiariki
- Region 3: Te Tauraki – Te Waipounamu/Rakiura, Wharekauri
- Region 4: The Cause Collective – Pasifika families nationwide
To find out more click HERE.
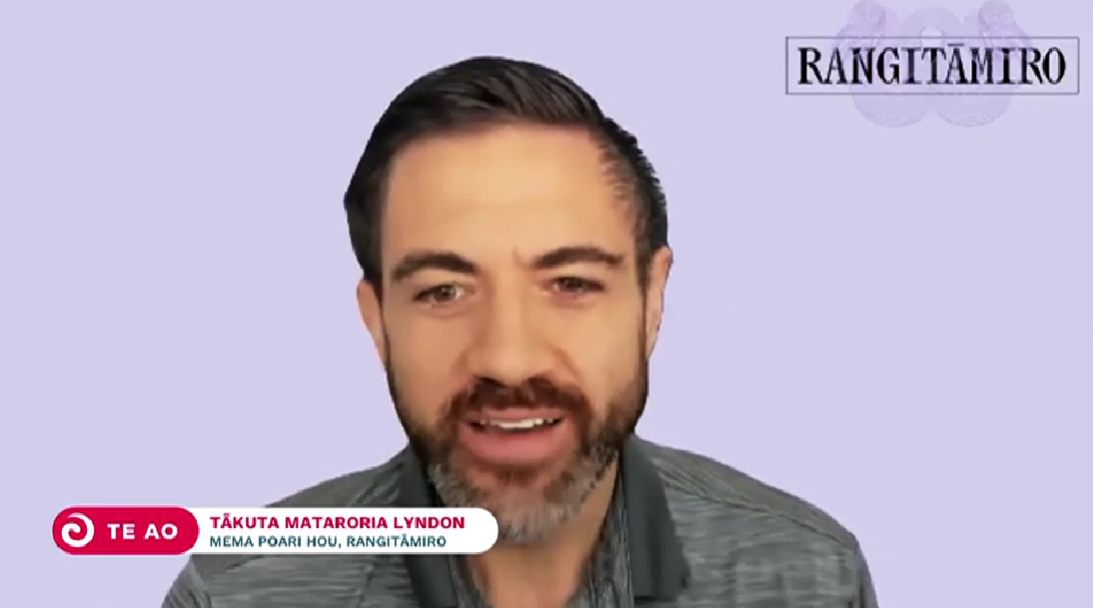
Dr Mataroria Lyndon, member of Te Tiratū Iwi Māori Partnership Board
Hauora at home: Everything under one roof in Whaingāroa
Poihākena Marae in Whaingāroa Raglan was the place to be this week as whānau gathered hauora check-ups, hosted by Toi Oranga in partnership with a range of local and visiting health providers. The open-door event invited whānau to drop in, share a cuppa, and check up on their wellbeing — all in a familiar, friendly environment.
Nurses were onsite offering general health checks, alongside a wide range of services including physiotherapy, mirimiri (traditional Māori bodywork), immunisation, cervical screening, and counselling. A Ministry of Social Development (MSD) staff member was also available.
Two Heart Foundation representatives were kept busy with blood pressure checks, while a local GP provided full consultations in a dedicated clinical space.
Having services close to home made a big difference, particularly for kaumātua who often face challenges accessing care, and for younger whānau looking for convenient, supportive options.
“Whānau felt more comfortable at the marae, and not having to travel far — and having everything under one roof in such a friendly space just made sense,” said Megan Tunks, one of our Whānau Voice kaimahi.
Predominantly Māori came, but some non-Māori as well. “They relaxed with a hot drink and some kai, connected with others, and visited different service providers while they waited.”
Many of the visiting providers, including the physiotherapist and mirimiri practitioners, were from the local community themselves — a powerful reminder of the strength and value of community-led solutions.
The kaupapa was simple and effective: bring health services to where whanau already feel safe, respected, and connected. The result? A whānau-first day grounded in manaakitanga, kaitiakitanga, and whanaungatanga— showing what’s possible when hauora is delivered with aroha.
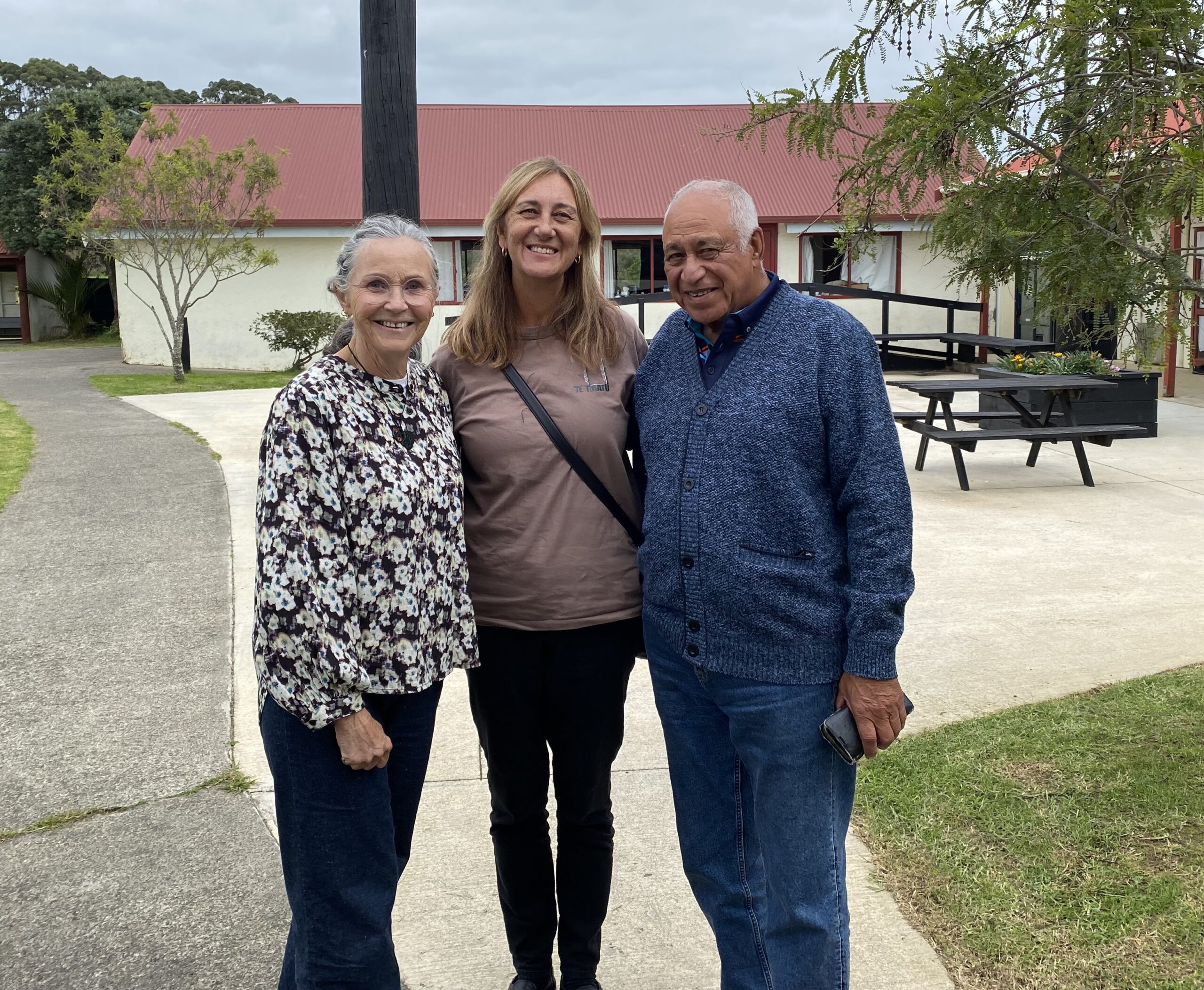
Photo: Lesley Thornley, a physiotherapist and daughter of the late Dr John “Digger” Penman, who served as the local GP from the 1940s to the late 1960s before being succeeded by Dr Ellison; Megan Tunks, Whānau Voice kaimahi with the Te Tiratū Iwi Māori Partnership Board; and Pablo Rickard, affectionately known as Whāingaroa Raglan’s ‘unofficial Mayor’.
From the Frontlines at Waahi Whaanui: Mental Health and Addiction Gaps
On the frontlines of whānau support, the cracks in the system are becoming impossible to ignore.
This week, our Whānau Voice team visited Waahi Whaanui in Raahui Pookeka-Huntly that was established in 1983 by the Tainui Maori Trust Board as one of its ten Marae Cluster Management Committees that works across a vast rohe — from Mercer in the north, to Raglan in the west, Te Hoe in the east, and Kirikiriroa in the south.
They deliver an impressive range of integrated services: Whānau Ora, parenting support, family violence response, social workers in schools, rangatahi transition services, alcohol and addiction support, and more. Deeply embedded in their hapori driven by a commitment to uplift whānau. But even with all their expertise, one reality stood out: they’re doing critical mahi with our people experiencing a health system under immense strain. The need is growing significantly, particularly for our rangatahi.
Mental Health: Access Denied by Distance and Delay
For Raahui Pookeka based whānau,often access mental health assessment is to travel half an hour to Hamilton. Once seen, they’re referred back to local services in Raahui Pookeka—services that are already under immense pressure.
The latest data from Te Hiringa Mahara – Mental Health and Wellbeing Commission backs this up:
- 16,000 fewer people were seen by specialist services in the year to June 2024, compared to 2021.
- More than 10,000 of them were under 25 years old.
- The drop isn’t because fewer people need help—it’s because they can’t get it.
This is a crisis. Not just of access, but of dignity.
Addiction Support Has a Waitlist—But Pain Doesn’t Wait
There’s a four-week wait to see an addiction counsellor at Waahi Whaanui. For some whānau, that’s a tipping point. There is limited alcohol and drug support for rangatahi under 18. We heard that many rangatahi are in crisis, with no place to turn.
Kaumātua Saving Up Their Pain
Kaumātua said they “save up” their health concerns because of cost and not wanting to be hōhā or overburden already stretched services.
It is not tika that they should feel like a burden. They carry our whakapapa, our mātauranga, our mauri. They should be cherished and prioritised.
The Numbers Are Stark—But Not New to Us
Māori in Waikato are:
- 9 times more likely than non-Māori to be hospitalised for any mental or substance use disorder
- 6 times more likely for schizophrenia
- 7 times more likely for substance and alcohol-related harm
- And an average of 225 Māori (mostly wāhine) are hospitalised for intentional self-harm each year
In Hamilton, over 2,000 Māori aren’t enrolled with a GP—shut out from the most basic preventative care.
Where to From Here?
What we saw was a failure of the health system to support providers like Waahi Whaanui who are under pressure, the increased caseload of kaimahi carrying too much without the resources they need, and whānau trying to hold on without falling through the cracks.
We stand alongside them—and we raise their voices.
Last week the Government announced a $28 million investment over four years in Budget 2025 to shift the response to 111 mental distress calls from Police to mental health professionals. For frontline providers like Waahi Whaanui it will take far more to address the deep gaps in accessibility, workforce, and culturally grounded care.
Te Tiratū is calling for:
Providers to be adequately resourced to cope with the increasing demand on services
- A focus on services for rangatahi under 18 that are locally relevant and accessible
- Appropriate whanau orientated triage processes
- Culturally grounded, local solutions led by whānau, hapū and iwi
Te Tiratū will continue to amplify your voice until the system listens.

From left to right: Rawinia Marsh – Integrated Services Manager Waahi Whaanui Trust, Fiona Helu and Hemi-Lee Morgan – Whānau Ora Team.
BUDGET 2025: Te Tiratū Iwi Māori Partnership Board: Uncompromising call to Govt on Budget 2025

The Te Tiratū Iwi Māori Partnership Board, the statutory voice for 114,000 whānau Māori across the central North Island, is issuing an uncompromising call to the Government: make Budget 2025 a decisive turning point so the health system is timely and accessible.
Maniapoto rising: “We know what works”
Our Whānau Voice kaimahi and Tumu Whakarae attended a recent hui held at Te Kūiti, hosted by Maniapoto Marae Pact Trust where a strong and heartfelt kōrero unfolded about the state of hauora for whānau across the Maniapoto rohe.
Frontline kaimahi, whānau navigators, and community leaders — including CEO Shirley Turner — came together to shine a light on what’s working, what whānau are asking for, and where the system is falling short.
“Our people know what works — we just need the system to back us,” Shirley said.
Maniapoto Marae Pact Trust offers a suite of integrated health and social services designed to walk alongside whānau, ensuring every door is the right door. These include:
- Kaiārahi Services – placing whānau at the centre, helping them define and lead their own goals across multiple service areas.
- Whānau Direct – offering fast, flexible support when whānau need it most.
- Disability support and mental health services, including social workers in schools.
- Tamariki Ora – a standout success story. The Tamariki Ora nurse and whānau navigator work together in the community, achieving strong immunisation rates despite not receiving equitable funding.

Photo from left to right: Te Tiratū Tumu Whakarae, Brandi Hudson with kaimahi of Maniapoto Marae Pact Trust – Sauaga Poliko, Lisa Kerekere, Rena Morgan, Honour Muraahi, Adrianna Astle and Raven Torea our Whānau Voice kaimahi
The Trust also contributes to Healthy Families Te Kūiti, with locals like Michelle Wi running weekly Māra Kai workshops on preserving, pickling, and food sovereignty — all part of a wider push for long-term wellbeing.
Shirley was clear about how the Trust works, “Whānau are in the driver’s seat — and that’s how it should be. Our services walk with them, not ahead of them.”
Systemic Challenges Undermining Equity
Despite these local strengths, systemic failures continue to undermine outcomes for Maniapoto whānau.
One striking example shared at the hui was of a kuia who was rushed by ambulance to Waikato Hospital with minimal belongings, only to be sent home later in a shuttle and left on the roadside.
It was only thanks to a member of the public contacting a local health worker that she made it home safely. This case highlights the urgent need for a more responsive, automatic travel support process — particularly around the National Travel Assistance (NTA) scheme.
“There needs to be a built-in, automatic system for whānau travel vouchers — not an afterthought.”
Other systemic concerns raised include:
- Falling through administrative cracks in post-hospital care and transport.
- No sustainable funding model for high-performing but underfunded services like Tamariki Ora.
- The need for better wellbeing measurement tools that reflect whānau realities.
- A desire for more regular, locally based specialist outreach, especially for kaumātua and kuia.
Networks and Ngā Kaupapa o te Rohe
The hui also acknowledged the strength of local collaborations — such as the Waitomo Community Health Forum and initiatives like Harvest to Home and Wai to Kai, which focus on food resilience, sovereignty, and wellbeing.
The message from Maniapoto is clear: local, kaupapa Māori solutions are working — but they need resourcing and system-level support.
“We’re seeing positive outcomes because our services reflect the lived reality of our whānau. But without equity in funding and process, our people continue to carry the cost,” said one kaimahi.
Uncompromising call to govt on Budget 2025
MEDIA STATEMENT
FOR IMMEDIATE RELEASE
22 May 2025, 12:00 PM
2 minutes to Read

[Photo: Tipa Mahuta and Hagen Tautari, co-chairs of Te Tiratū Iwi Māori Partnership Board]
The Te Tiratū Iwi Māori Partnership Board, the statutory voice for 114,000 whānau Māori across the central North Island, is issuing an uncompromising call to the Government: make Budget 2025 a decisive turning point so the health system is timely and accessible for whānau.
The Board is calling for urgent action and bold direct investment in Māori-led, community-based health services — warning that failure to do so will mean continued whānau premature death from preventative disease, entrenched hardship and inequity across the rohe.
Board co-chair Hagen Tautari said, “We hear it from our people every day — the system is not meeting the needs of our whānau who top the table in terms of mortality and morbidity statistics.”
He acknowledged steady progress in key service areas — particularly newborn enrolment, early intervention, and screening coverage across the Tainui Waka rohe. However, he stressed that falling immunisation rates and long specialist wait times now demand urgent attention.
“Whānau are waiting months — even years — for essential care. Many needing to access services beyond a GP clinic are forced to travel vast distances, bear unaffordable costs, or give up altogether because the system isn’t designed for them — culturally, practically, or equitably. It’s not just unjust — it’s deadly. This failure is costing lives.”
Evidence from Whānau Voice surveys, the Board’s monitoring mechanism on Te Whatu Ora Health New Zealand reveals that Māori communities across the Te Tiratū region — spanning from Waikato to Hauraki, from Te Kuiti to Kawhia and especially the surrounding rural settlements — continue to face persistent, systemic failures in accessing even basic health care.
“Since June 2023, I’ve been on a waitlist for gallbladder surgery. This one condition is stopping me from getting back to work,” said one Tokoroa-based whānau. “My partner needed someone to talk to. There was no mental health support for him. Nothing,” shared another. “As a teacher here in Tokoroa, I don’t think there’s enough on offer for our tamariki in terms of mental health.”
Tautari believes these stories are not isolated — they are representative of widespread experiences shared by whānau across the rohe that are leaving them frustrated, overlooked and unsure on where to get help.
Even the government’s recent pre-announcement of a funding boosts for 24-hour urgent care in selected locations, Ōpōtiki—part of the Te Manawa Taki region where Te Tiratū operates—was overlooked despite having a clear need and geographic isolation. As a result, the lack of accessible services continues to place whānau lives at risk.
The resounding call from the flaxroots is clear: more GPs, more specialists, shorter wait times, and longer appointments. “We need to be able to see a doctor the same day — not in two weeks. You could be dead by then,” said whānau from rural Waikato.
Te Manawa Taki Central North Island Region: Delays, Disconnection, Causing Disadvantage
Whānau in the Te Tiratū catchment compared to the general population continue to face higher rates of cancer, diabetes, mental health conditions, and preventable illnesses — with poorer outcomes and shorter life expectancies.
These outcomes are worsened by the current service delivery experience:
- Surgery and specialist waitlists stretching months to multiple years
- Lack of local mental health support especially for tāne and rangatahi
- Shortages of GPs and specialists in rural and coastal communities
- Disjointed services that are not designed to reflect Māori cultural values, realities, or aspirations
From rural towns like Putāruru and Mangakino to coastal Ōpōtiki, many whānau struggle to access timely, affordable, and culturally safe health care. Services are stretched, under-resourced, and often located far from where whānau live.
- Teachers in Tokoroa are concerned about the lack of mental health services for students even though suicide rates for rangatahi are among the highest globally, and tamariki are more likely to experience barriers to accessing mental health services.
- Te Whatu Ora data for the Te Tiratū region indicates more whānau are now waiting over 4 months for their first specialist appointment. Delays in accessing timely care especially for rural and remote areas is worsening the health conditions for whānau and eroding their trust in the system. As a result, many are disengaging entirely — avoiding the very services meant to support them.
- In the western Bay of Plenty, whānau report long waits for referrals and specialist treatment in Hamilton, often delayed by transport, time off work, or simply unaffordable travel.
“Referrals wait times are really long!” said whānau. “We need doctors full-time — the same doctor, not locums that come and go,” said another.
Many reported being bounced between services, without follow-up, clarity, or support. “We’re constantly referred elsewhere. No one checks in. The system is disconnected, and people as a result fall through the cracks.”
Decades of Underinvestment: Now a Measurable Impact
This crisis is not new. Back in 2019 the Waitangi Tribunal released its Hauora Report on WAI 2575 matters that was further supported by the historic Sapere Report that calculated a $531 million longstanding underfunding experienced by Māori providers which still has not been addressed and compounding – six years later.
While Te Tiratū waits for the official details of the Budget 2025 commitments— such as a proportion of the allocated $6.8 billion capital spend on health and what the $190 million Social Investment Fund entails— there is no assurance that these will reach Māori communities unless targeted, ringfenced, and co-designed.
Te Tiratū urges the Government to:
- Deliver dedicated investment into kaupapa Māori and whānau-centred health models
- Address workforce shortages in GPs, mental health specialists, and kaiārahi/navigators across the rohe
- Guarantee equitable access to timely mental health care care for tamariki, rangatahi and tāne
- Uphold Te Tiriti o Waitangi in health system governance and decision-making
“What works for our whānau already exists. We just need the government to invest in it — as Māori-led care can deliver,” said Tipa Mahuta, co-chair of Te Tiratū Iwi Māori Partnership Board.
A local initiative already making a measurable difference is a community outreach pilot launched by BreastScreen Aotearoa, in partnership with Hauraki PHO, to connect under-screened wāhine through hospital and community pathways.
Equity Is Not a Luxury — It’s a Legal and Moral Obligation
Te Tiratū Iwi Māori Partnership Board believe whānau Māori across the Tainui waka rohe cannot afford more delays, trade-offs, or one-size-fits-all approaches.
“Equity is not optional — it is a Treaty commitment, and the path forward to sustainable wellbeing. Now is the time for genuine partnership — one that shares power, resources, and responsibility with Māori to achieve oranga for all.”
Rangitāmiro leads the way – First Commissioning Agency to complete Whānau Ora procurement process
PANUI FOR WHĀNAU ORA PROVIDERS
IN TĀMAKI MAKAURAU & TE TAI TOKERAU
21 May 2025, 6:00 PM
2 minutes to Read
Rangitāmiro is proud to announce that it has successfully completed its inaugural Whānau Ora procurement process and today formally notified successful providers across Region One. This is a significant milestone and reaffirms a commitment held by Rangitāmiro to honour the whakapapa of whānau ora through strengthening service networks, regional capability, reach and service coverage, ensuring and enabling whānau wellbeing.
A comprehensive and values-led procurement process that interim Rangitāmiro Chair, Dr Rachel Brown knows will shape the future of Whānau Ora delivery.
“We are honoured to be able to give providers and communities across Aotearoa confidence in the continuation of Whānau Ora services with minimal disruption, whilst ensuring growth in capacity means service reach and coverage will increase allowing more whānau to access the services they need.
Key achievements from this process include:
• Guaranteed continuity of services for whānau from 1 July 2025, with proactive steps to minimise transition disruption
• An increase in frontline Kaiwhiriwhiri Whānau FTE, supporting a stronger navigation workforce across all regions
• Expanded reach into isolated and rural communities, enabling better access to culturally anchored, whānau-centric support
• The onboarding of new providers, bringing fresh innovation, insight, and presence in areas where service gaps previously existed
Dr Brown acknowledges the tenacity of providers and whānau in the short timeframe.
“Today’s announcement signals the next chapter in our partnership with whānau and reinforces our long-term commitment to the transformation and future of Whānau Ora. Our kaupapa is grounded in empowering whānau, driving better outcomes, and expanding service reach to underserved and high-need communities.”
Rangitāmiro is a collaborative entity comprised of Te Tiratū Iwi Māori Partnership Board, the National Hauora Coalition, and Ngaa Pou Hauora oo Taamaki Makaurau Iwi Maaori Partnership Board.
National immunisations up as Māori rate treads water

An uptick in overall immunisation rates for infants and young children is to be welcomed, but rates for tamariki Māori continue to lag, says Mataroria Lyndon.
The University of Auckland senior lecturer and member of Te Tiratū iwi Māori partnership board says it is important to recognise progress has been made, “but that does not necessarily reflect the reality for Māori and inequity”.
National immunisation rates climb, but Māori communities still lag behind
Te Tiratū Iwi Māori Partnership Board member Dr Mataroria Lyndon MBCHB, MPH, PHD said national statistics, while encouraging, fail to reflect the challenges Māori continue to face.
“I want to whakanui and recognise that that’s important, that we are making progress,” he said. “But, we know that those national rates don’t reflect the realities for Māori and the inequities or the gaps around Māori immunisation rates, which are sitting at 62% in our rohe of Waikato-Tainui, and I know it’s similar for Te Tai Tokerau as well.”
Dr Lyndon is urging the health system to respond with equity at the centre — supporting Māori-led initiatives, breaking down access barriers, and building trust through culturally grounded communication.
Because protecting all tamariki means ensuring every child, in every community, has the same opportunity to be safe and well.