Associate Health Minister with responsibility for Rural Health, Matt Doocey and Minister for Rural Communities, Mark Patterson came to Thames today, to hear directly from the frontline about the challenges facing rural communities.
Doocey set out the five priorities of the Rural Health Strategy; recognising rural communities as a priority group, focusing on prevention for a healthier future, ensuring services are available closer to home, supporting access to services at a distance, and building a valued and flexible rural health workforce.
He also noted the review underway of the travel assistance programme, ongoing workforce pressures, and the rollout of one of six prototype digital telehealth services, with Thames chosen as a pilot site for 24/7 support.
While government priorities were outlined, much of the kōrero centred on the lived realities of staff, communities and a Māori provider of affordable health and wellness services across the Hauraki rohe for over 25 years.
Attendees described severe burnout among doctors and nurses, with calls for immediate workforce relief in Hauraki. Many emphasised that the bulk of the health workforce are women, yet parity in pay remains unresolved, creating inequity and undermining retention.
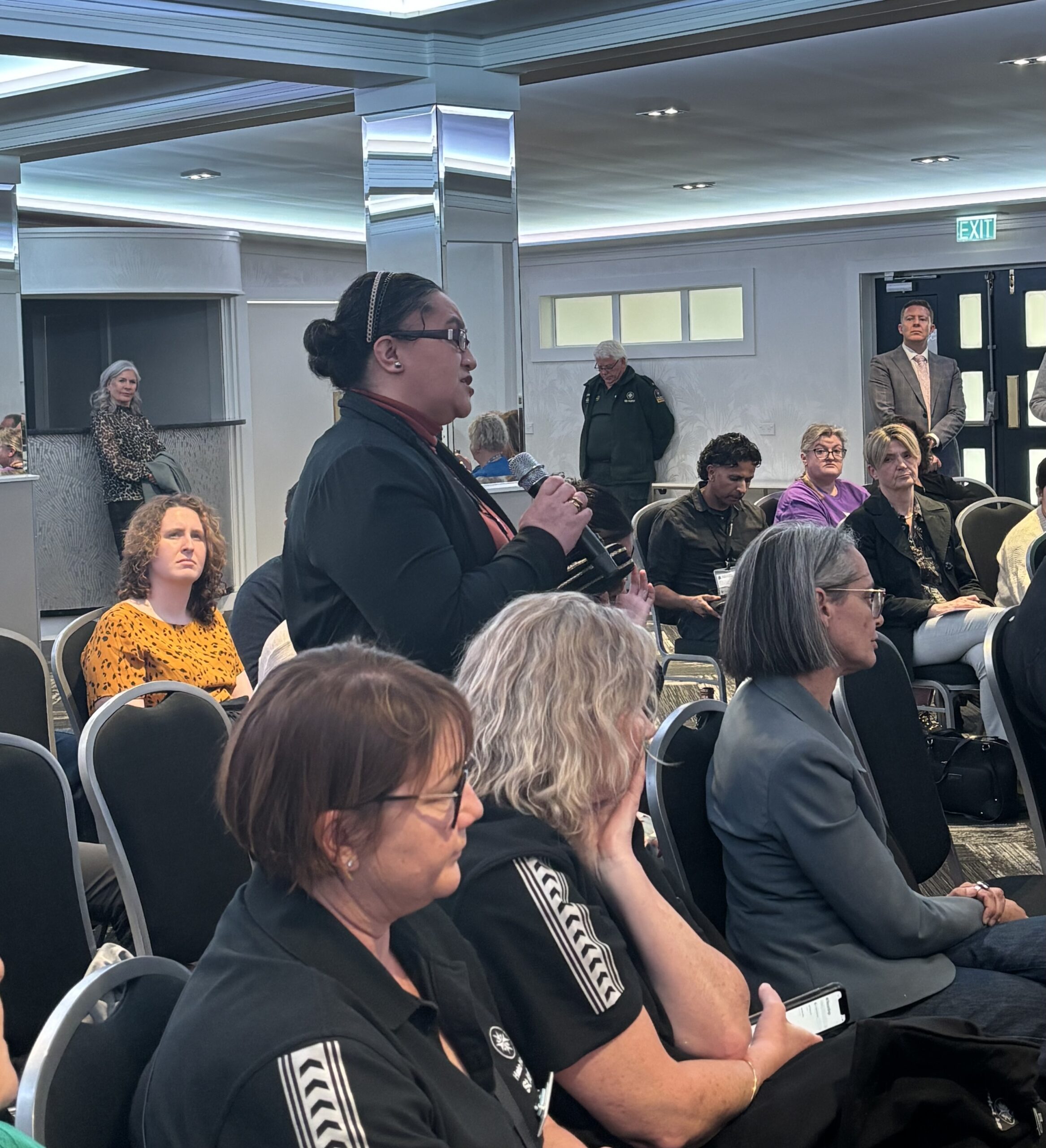
CEO of Te Korowai Hauora o Hauraki, Tammy Dehar, stood to share whakaaro about what integrated services might look like if they included the social determinants of health. She urged government to design solutions with communities rather than impose top-down targets, especially to support rangatahi. Similar calls were made for better training pathways, with regulated health body training and youth development identified as vital to the future of the rural health workforce.
Rural GP Alex McLeod also spoke out, saying good primary care services are not being given enough regard in government health design and resourcing. He said kaupapa Māori providers already deliver effective, whānau-focused care but are undermined by fragmentation and competition for funding. He urged government to consider local governance for primary care, rather than allowing secondary services to dominate leadership and decision-making.
In response, Doocey said immigration and skilled migration could help to address workforce shortages but were “not a silver bullet,” with policy settings needing to shift. He confirmed that a new mental health crisis response service is being developed with Police over the next three years and acknowledged the importance of building equity into workforce planning. A senior nurse and a nurse practitioner have also just been approved for the Thames Hospital ED.
Housing emerged as another barrier, with limited supply making it difficult for staff to stay and live locally. Safety was also raised, with communities dealing with domestic and sexual violence, drugs and alcohol, and the resulting rise in mental distress. Without adequate supports, attendees said, these pressures compound the crisis for both whānau and frontline services.
Transport and access challenges were highlighted, especially for elderly residents. After-hours services remain very limited. A short-term transport option provided by Thames Hospital earlier this year was welcomed but is not permanently funded. Seasonal pressures also weigh heavily, with the summer population in Coromandel surging from around 1,400 residents to 30,000 visitors, stretching an already fragile system.
In Waihi, residents face a three-day wait for telehealth services, with no permanent local health professionals and reliance on Thames Hospital ED. While Te Whatu Ora has committed to changes, attendees said stronger support for rural health practitioners is essential.
The hui also heard about local innovations such as the Colville Project, promoted and led by Dr Katie Armstrong, which integrates housing solutions, youth trainee pathways, and visiting specialist support. With $1.29 million already raised, the project demonstrates the ability of rural communities to design and deliver their own solutions when adequately supported.
The meeting showed that rural health cannot be transformed without resourcing the workforce, addressing housing and pay equity, and empowering local solutions that reflect the realities of rural communities. As Minister Doocey acknowledged, co-design and localism must sit at the heart of the Rural Health Strategy if it is to deliver for Hauraki and beyond.